Please view our updated COVID-19 guidelines and visiting procedures →.

Hallucinogens, used in psychiatric practice in the 1950s and 60s for the treatment of addiction, alcoholism, depression, and other disorders, were designated as Schedule 1 – illegal – under the Controlled Substances Act in 1970.
While still federally illegal in 2025, these substances have reemerged as promising therapies for the management of a variety of psychiatric illnesses and in end of life care.

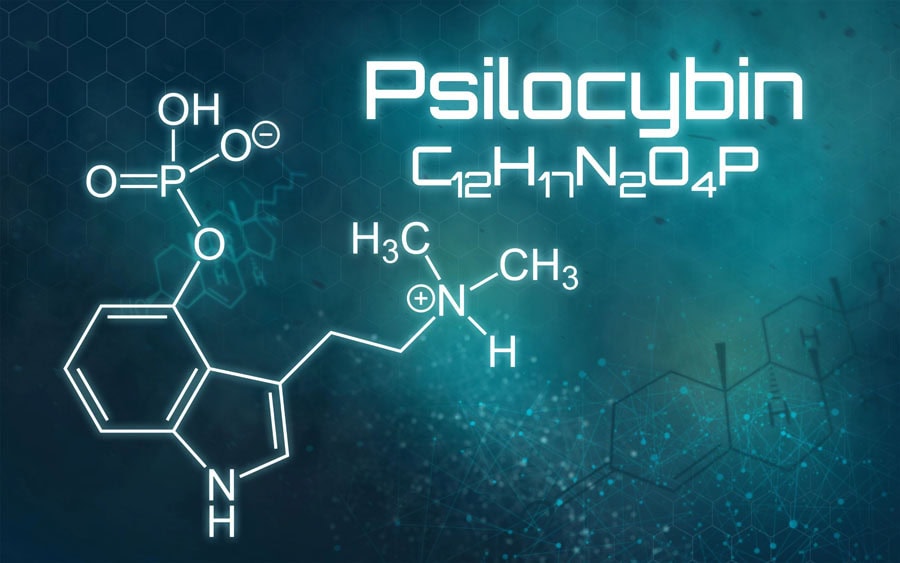
Psilocybin, the active ingredient in “magic mushrooms,” has shown positive outcomes in terminal cancer patients and those with other life-limiting conditions, particularly in patients struggling with existential distress, anxiety, and depression in advanced illness.

While beyond the scope of this blog, the basic mechanism underpinning the therapeutic benefits of hallucinogens is believed to involve the agents’ ability to increase “neural plasticity” in the brain—especially regarding long-held personal beliefs. These preexisting, “hard-wired” neural pathways (the so-called “Default Mode Network”) define an individual’s memories and plans, role and place in the world, interpersonal relationships, and other traits central to the ego, or sense of self.
People using hallucinogens often describe a dissolution of the ego, resulting in a broader sense of belonging or even merging with nature, other people, and the universe. They report a quieting of the internal narrator (“I am defined by this, my role is to do that”).

People using psilocybin at the end of life—particularly those questioning the meaning and value of their lives and fearful of ceasing to exist—may redefine death not as an ending, but as a process of transition to something eternal or interconnected.
Many also find deep spiritual meaning, regardless of religion, a sense of peace, emotional catharsis, and a belief that consciousness and love transcend death.
Several studies have been conducted using psilocybin in seriously ill patients and those at the end of life:
It is important to note that these outcomes are not guaranteed. “Ego death” can be terrifying if a person is unprepared.

Psilocybin is currently not a part of the CT Hospice formulary. However, as research in the field progresses—presumably showing salutary effects of this hallucinogen in patients at the end of life—it may become a more commonly used drug (assuming it becomes legal!) in our never-ending quest to improve end of life care.

As a not-for-profit, we depend on generous donors to help us provide customized services and therapies that aren’t completely covered by Medicaid, Medicare, or private insurance.
Please make a gift to help us sustain the highest standard of care.
Admissions may be scheduled seven days a week.
Call our Centralized Intake Department: (203) 315-7540.