Hospice care is a specialized form of healthcare that focuses on enhancing the quality of life for individuals with terminal illnesses. The goal is to provide comfort, support, and dignity during the end-of-life journey. However, the use of medications, particularly benzodiazepines, have been both a blessing and a controversy in end-of-life care. In this blog post, we will explore the role of benzodiazepines in hospice care, the benefits they offer, potential drawbacks, and the ethical considerations surrounding their use.
Understanding Benzodiazepines
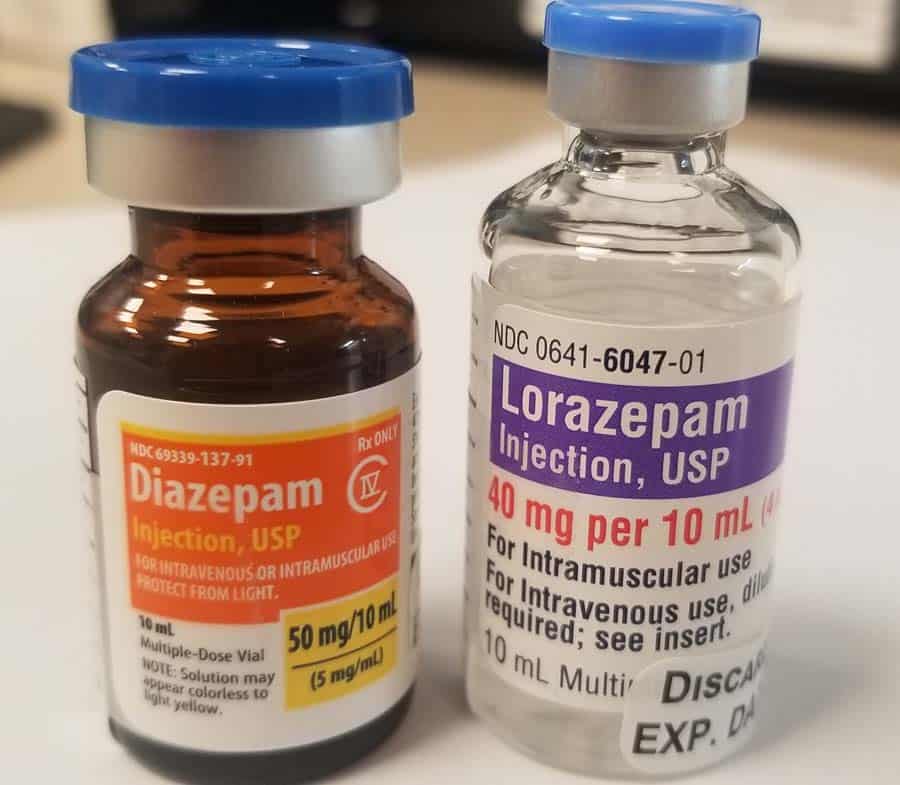
Benzodiazepines are a class of sedative drugs that act on the central nervous system. They are commonly prescribed to alleviate symptoms such as anxiety, insomnia, and seizures. These medications produce a calming and sedative effect. Examples of benzodiazepines include diazepam (Valium), lorazepam (Ativan), and alprazolam (Xanax). While these medications can be highly effective in managing certain conditions, their use in hospice care requires careful consideration.
Benefits of Benzodiazepines in Hospice Care:
- Anxiety and Agitation Management: One of the primary benefits of benzodiazepines in hospice care is their ability to manage anxiety and agitation. Patients facing terminal illnesses often experience heightened stress and restlessness. Benzodiazepines can provide relief, promoting a sense of calm and comfort in the final stages of life.
- Insomnia Relief: Terminal illnesses can disrupt sleep patterns, leading to insomnia. Benzodiazepines may be prescribed to help patients sleep more soundly, contributing to an improved overall quality of life during their remaining time.
- Seizure Control: For individuals with terminal conditions that may involve seizures, benzodiazepines can be crucial in controlling and preventing these episodes. This can significantly enhance the patient's comfort and reduce distress.
- Symptom Management in Respiratory Distress: In cases where respiratory distress is a prominent symptom, benzodiazepines can help relax the respiratory muscles, making breathing more comfortable for the patient.
Potential Benzodiazepine Drawbacks and Concerns:
- Sedation and Cognitive Impairment: A common concern with benzodiazepine use in hospice care is the potential for sedation and cognitive impairment. While these effects can be beneficial in managing symptoms like anxiety, sedation may hinder the patient's ability to interact with loved ones or communicate effectively.
- Risk of Withdrawal and Tolerance: Prolonged use of benzodiazepines can lead to tolerance, in which a medication becomes less effective over time, making higher doses necessary for the desired effect. Symptoms such as increased anxiety, jitteriness, or -- in rare circumstances -- seizure can result from abruptly stopping these medications, but is rarely a concern in hospice patients, in whom their cessation is unusual.
- Respiratory Depression: Benzodiazepines, particularly in combination with other medications, can contribute to respiratory depression, a possible concern in patients who already have compromised respiratory function. Expert, judicious use of these medications – essential for the relief of anxiety and air hunger in patients at the end of life– by experienced hospice physicians mitigates this risk.
- Communication Challenges: Side effects such as sedation and cognitive impairment that may be unexpected by the families and loved ones of hospice patients can create misunderstanding between healthcare providers, patients, and their families. Clear information as to each patients goals of care and the use of these medications becomes vital to ensure that the patient's wishes and concerns are understood and addressed.
Other Benzodiazepines Considerations:
The use of benzodiazepines in hospice care requires thoughtful reflection. Key considerations include:
- Patient Autonomy: Respecting the autonomy of the patient is paramount. Healthcare providers must engage in open and honest discussions with patients, involving them in decisions about their care and the use of medications.
- Balancing Symptom Relief and Quality of Life: Striking a balance between providing symptom relief and maintaining the patient's quality of life is paramount to hospice care. The experienced hospice professionals at Connecticut Hospice are expert in weighing the benefits and risks of benzodiazepine use, and considering the individual needs and preferences of each patient.
- Informed Consent: Informed consent is crucial in hospice care, including education about the benefits and risks of benzodiazepine use. Patients and their families should be well-informed to make decisions aligned with their values and goals.
- Regular Reassessment: Regular reassessment of the patient's condition is essential to ensure that the benefits of benzodiazepine therapy continue to outweigh potential risks. Adjustments to the treatment plan may be necessary based on the evolving needs and circumstances of the patient.
Benzodiazepines in Palliative Sedation:
Palliative sedation is a carefully regulated and monitored medical intervention that is employed when other forms of symptom management have proven ineffective. It is typically reserved for patients experiencing severe distress, refractory symptoms, or existential suffering that cannot be alleviated through conventional means. Palliative sedation aims to balance the relief of symptoms with the preservation of patient comfort and dignity. Benzodiazepines, a class of sedative drugs, are frequently employed in palliative sedation due to their effectiveness in promoting a peaceful and comfortable experience for patients nearing end of life.
The use of benzodiazepines for palliative sedation in hospice care is a complex but widely ethically accepted practice. These medications offer effective symptom control and rapid onset of sedation, and their use requires careful consideration of individual patient needs, open communication, and adherence to ethical practice – long a core principal of patient care at Connecticut Hospice. The goal of hospice physicians who employ palliative sedation is always the enhancement of patient comfort and dignity during the final stages of life. By embracing a patient/family-centered, multidisciplinary approach, healthcare professionals can provide compassionate care that honors the values and preferences of those under their charge, ensuring a peaceful and dignified journey toward the end of life.
Best Benzodiazepine Practices and Guidelines:
- Individualized Care Plans: Tailored Approaches: Recognizing that each patient's experience is unique, hospice professionals should develop individualized care plans, considering the specific symptoms, medical history, and preferences of the patient.
- Multidisciplinary Collaboration: Team Approach: A multidisciplinary approach involving physicians, nurses, social workers, and other healthcare professionals is essential. Regular team discussions can help assess the ongoing need for benzodiazepines and adjust treatment plans accordingly.
- Regular Reassessment: Ongoing Evaluation: Given the dynamic nature of hospice care, continuous reassessment of the patient's condition and response to benzodiazepines is crucial. Adjustments to medication regimens should be made based on the evolving needs of the individual.
Common Benzodiazepines:
Alprazolam
- Common Brand Name - Xanax
- Onset of Action - Intermediate (1-2 hours)
- Half-Life - Short (12 hours)
- Potency - High
- Metabolism - Hepatic
Lorazepam
- Common Brand Name - Ativan
- Onset of Action - Intermediate (1-2 hours)
- Half-Life - Intermediate (12-18 hours)
- Potency - High
- Metabolism - Hepatic
Diazepam
- Common Brand Name - Valium
- Onset of Action - Intermediate (1-2 hours)
- Half-Life - Long (20-100 hours)
- Potency - High
- Metabolism - Hepatic
Clonazepam
- Common Brand Name - Klonopin
- Onset of Action - Intermediate (1-2 hours)
- Half-Life - Long (18-50 hours)
- Potency - High
- Metabolism - Hepatic
Temazepam
- Common Brand Name - Restoril
- Onset of Action - Intermediate (1-2 hours)
- Half-Life - Short (8-22 hours)
- Potency - Moderate
- Metabolism - Hepatic
Oxazepam
- Common Brand Name - Serax
- Onset of Action - Slow (2+ hours)
- Half-Life - Short (5-15 hours)
- Potency - Low
- Metabolism - Hepatic
Benzodiazepines in Hospice Care Conclusion:
The use of benzodiazepines in hospice care requires careful consideration of medical, ethical, and patient-centered factors by experienced physicians and nurses. These medications offer valuable benefits in managing symptoms associated with terminal illnesses; patients and families may be assured that the healthcare providers at Connecticut Hospice expertly navigate all potential concerns associated with their use. Open communication, informed consent, and regular reassessment are key components of a comprehensive approach to benzodiazepine use in hospice care, ensuring that the patient's final journey is characterized by comfort, dignity, and respect for their autonomy.