Please view our updated COVID-19 guidelines and visiting procedures →.
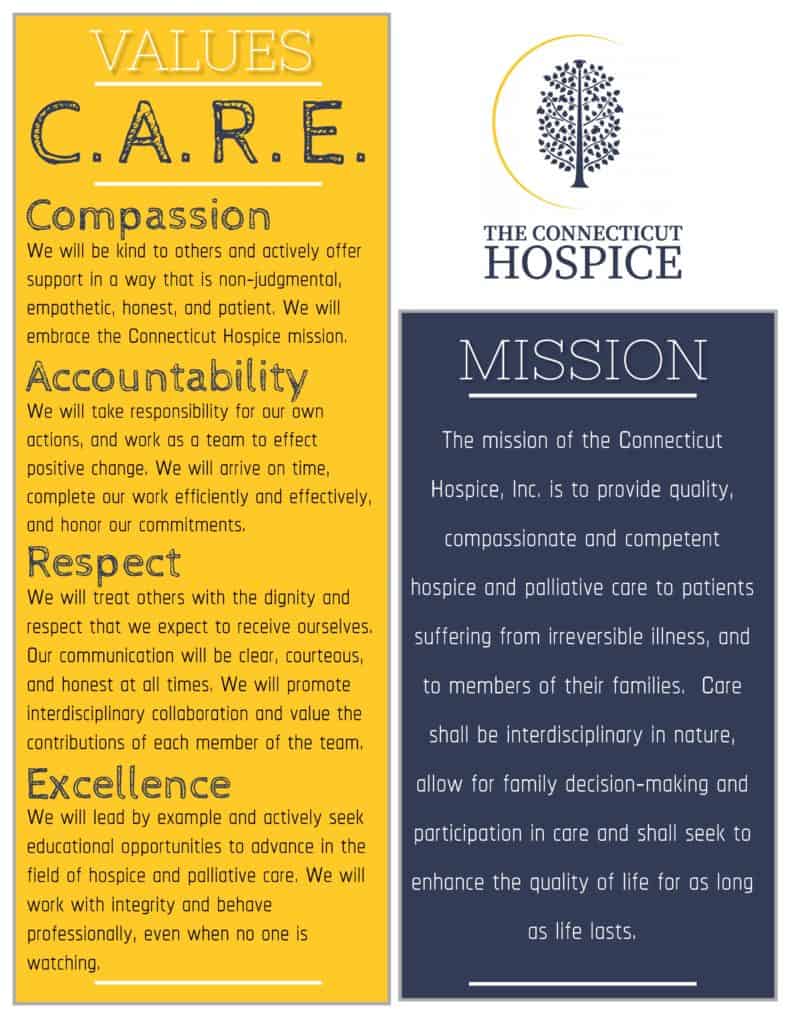
What makes Connecticut Hospice the right choice for hospice and palliative care? A staff that is guided by core values of C.A.R.E. to ensure the best in patient and family care. While a lot has changed since the start of Hospice in 1974, the quality of care provided has remained the same. In a recent new hire orientation, CEO, Barbara Pearce, stressed the importance of sharing not only the history and mission of The Connecticut Hospice to all new employees, but it is equally important to instill the guiding principles that all staff must follow to continue delivering the utmost quality of care: Compassion, Accountability, Respect, and Excellence (C.A.R.E.).
Beyond a shadow of doubt, the work that is done by each member of the Connecticut Hospice team matters and is valued by the organization as well as those impacted. Though quite frequently, when speaking with a Connecticut Hospice employee or volunteer, they will tell you that the work they do makes just as big an impact on their lives as those they care for.
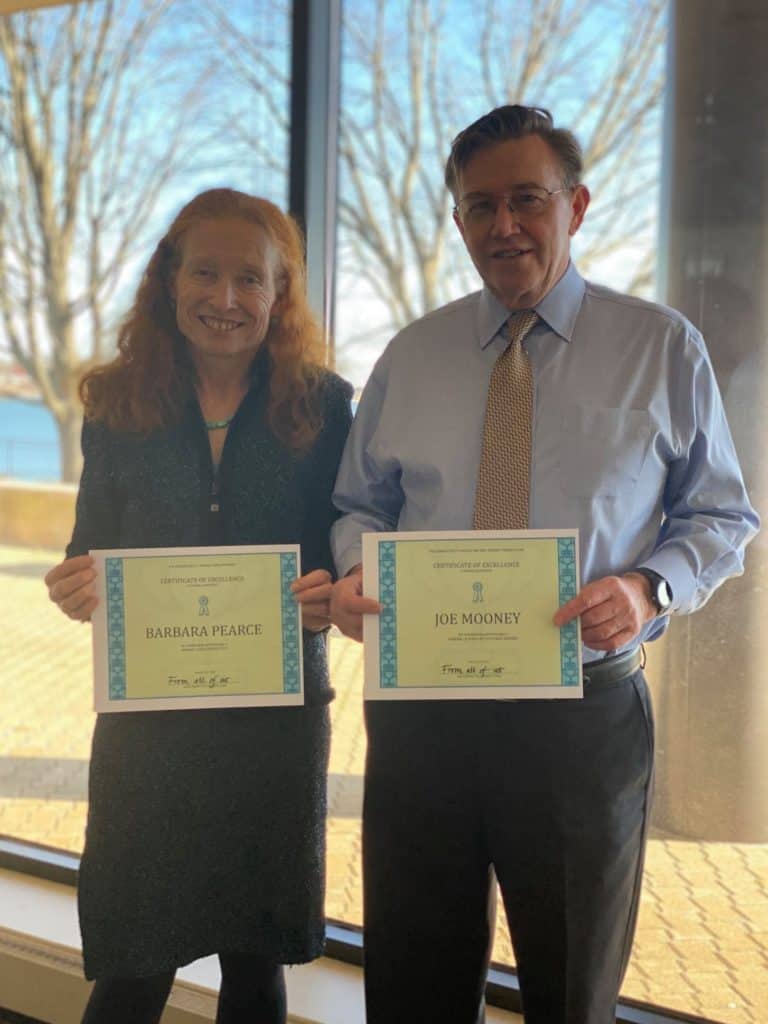
February 1, 2021 marked the 2nd anniversary of new leadership taking over The Connecticut Hospice. It was a relief for the staff when Barbara Pearce, CEO, and Joseph Mooney, CFO, arrived bringing hope for American's 1st Hospice. And, while it is no secret of the mountain of challenges and changes the non-profit has been through over the last two years, it isn't until you hear them spoken out loud that it becomes apparent that Connecticut Hospice is resilient.
In a recent interview, Barbara Pearce, CEO, shared her recollection of her last two years at Connecticut Hospice, with Bruce Tulgan, creator of The Indispensables podcast. Listening to Barbara share the numerous and sometimes grueling challenges the organization has faced during the last two years, it becomes clear why Connecticut Hospice has been around for forty-seven years -- hospice care started at and continues at Connecticut Hospice.
Use link below to hear the full podcast.
The Indispensables Podcast
Conversations with real go-to people who stand the test of time in the real world of work. Based on Bruce Tulgan's new book, The Art of Being Indispensable at Work, The Indispensables is a podcast series about how real people, in the real world, become indispensable, go-to people who stand the test of time at work. For more information, visit Rainmaker Thinking.
"Connecticut Hospice may not be able to add days to your life, but it can certainly add life to your days." -Barbara Pearce

When one enters The Connecticut Hospice, it becomes almost immediately clear what a nurse-centric place it is. There’s a reason for that, and her name is Florence Wald. She was our founder, often called the Mother of Hospice in America.
For many years, the nurses have asked for a picture of our founder on the inpatient floor. Through the good graces of two retired Connecticut Hospice nurses, Gen O’Connell and Dianne Puzycki, and portrait painter, Angela Rose Agnello, (daughter of staff nurse), we unveiled the portrait of Florence Wald on the second floor yesterday, to great applause.

We have written elsewhere about our history, and the long list of our accomplishments, but it’s important also to understand just how Florence Wald changed the care of patients with terminal illnesses. After she spent time at the world’s first hospice in London, Saint Christopher’s, she returned with determination to alter the course of end of life care.
At that time, in the early 1970s, people often wouldn’t even say the word “cancer” out loud. Some of you remember when it was referred to as the “Big C”. There were even those who feared that cancer could be contagious, and were afraid to be too close to those who had it. Of course, in those days, the likelihood of survival was much lower. Sometimes, doctors didn’t tell patients, or families, what the course of the disease would be, or that person’s prognosis. This led to people dying without closure, or with survivors only beginning to process their grief.
For all these reasons, Ms. Wald decided early on to focus on the care of cancer patients. She was a force of nature, and was determined to change what many doctors and nurses considered standard practice at the time. Researchers can read many of Florence Wald’s papers, thanks to the Yale School of Nursing.
Of particular concerns was what happened to those left behind, especially children of cancer patients. This might not be considered a good idea by many, but she got involved in the lives of the families, even taking some of the children home with her. She wanted them to have the comfort they weren’t getting in the medical system of that time.
Medicare set up what are now known as COP, Conditions of Participation, and they govern what hospice care needs to include. One of those requirements, 13 months of bereavement care for the survivors, is now practiced everywhere, and most likely came from those early principles espoused by Florence Wald.
Much of what we consider essential for death with dignity also harks back to those first patients. We now have a Plan of Care for everyone, and patients participate to whatever extent they can in planning for their end of life care. Doctors are now taught in medical school to have those difficult conversations, although many of them say that much more training is necessary. And, even though there is still a tension between the medical profession’s drive to keep patients alive, and the realities of the likely outcomes, we do see people choosing palliative care, when curative treatment becomes risky or speculative.
Cancer is not a verboten word anymore, but our tradition of treating the dying, no matter the cause, continues. We took wonderful care of AIDS patients in the early days of that scourge, and today we accept COVID-positive patients into our care. We try to give patients peace, comfort, freedom from pain, and closure, in whatever form that takes for them.

Florence would have been proud of us when we arranged for a dying man to say goodbye to his horse on our lawn, or when a social worker put another man’s feet into buckets of water pulled up onto his bed, so that he could feel the seawater one last time. Or, when a patient got to experience one last surprise birthday celebration, and share it with her family living on the other side of the country.

We are grateful for the wonderful legacy we have from Florence Wald and those early nurses who toiled alongside her. The world is a better place because of her work, and what better closure could there be to a life?

When my first daughter was born, a friend noted: “your capacity for grief has greatly and suddenly expanded.” And it had. The friendship, love, pride and the beauty of certain moments – whether or not we notice them in the moment -- are the fruits of our close relationships. As these treasures mount, so does the potential pain we will feel when suddenly that loved one is gone. As for me, I suppose my own capacity for grief has skyrocketed since that day – which also means there are more people (and a dog) in my life with whom I have strong and loving ties.
We observe mourning rituals because they are personally and culturally important and because we need a script to follow when we are in such unfamiliar territory. Those actions – funerals, wakes, shivahs, burials and unveilings -- represent our external, “public” expressions of loss.
We also have an internal experience, called grief. Unlike mourning, grief does not follow a timeline, or have an end date. Grief is often called a journey, and aptly so.
In one sense, we travel through grief as we experience its different stages, including the grief we start to feel even before the loss. Interestingly, the word “hospice” in medieval times referred to a way station for travelers . . . a place providing sanctuary for footsore and weary pilgrims.
Grief also feels like a constant companion – often a quiet one, sometimes disruptive, sometimes a comforting, and wholly unpredictable.
When my sister died I indeed paid the steep price of love. And I experienced grief as both the trip, and the companion. I have noticed the change in how I feel the pain, more a dull ache now than a sharp pain – and I have felt sad, even guilty and almost disloyal about that. That is the trip I am on.
I also have sudden realizations, like understanding that some of my memories were only shared between the two of us, that no one else would understand. Or that our common traits and quirks are now just mine. I think about how she would have handled pandemic times, what we would have decided about coloring our hair, and how we might talk about politics. Or I will stare at her photo and have a little conversation or a laugh. These make up the grief companion I travel with.
During this time of pandemic, the mourning and grief of the bereaved are layered with the tremendous emotional impact of current circumstances. Survivors of one who has died in isolation due to pandemic restrictions, may feel not only profound grief but also trauma from their loved-one’s rapid decline, their inability to comfort them, and not being with them as they died. Trauma is what happens in the brain when an individual experiences something that takes them beyond their normal emotional coping capacity. Experiencing trauma includes symptoms such as anxiety and flashbacks, and it interrupts the normal grief process.
I believe that many bereaved during these past months have, at best, a shaky foundation for moving through their grief. To those who feel unmoored and alone, I offer sincerest hope that they will find stability to start their journey, and happy memories to keep them company along the way.
The Bereavement Program at Connecticut Hospice is a resource for those bereaved who need grief support after the loss of a loved one under our care. It has become quite apparent that the grief that our bereaved are dealing with has been complicated by the COVID-19 pandemic. The fact is that many friends and family members, who were unable to visit their loved ones at all, due to the visitor restrictions for hospitals, nursing homes and assisted living facilities, had not seen their loved ones for months prior to admission to Connecticut Hospice in Branford. This has become part of the grieving process for many bereaved, unable to comfort their loved ones, or be the advocate at the bedside. The bereaved we are caring for are grieving what feels to be layers of emotion related to the unexpected crisis of the COVID pandemic in addition to the grief related to the death of their loved one. The Connecticut Hospice Bereavement Program continues to navigate this journey with the bereaved, providing comfort and support during a very difficult time, including group meetings. For more information, call Jennifer Stook, Director of Bereavement Services, at 203-315-7544 or visit www.hospice.com/bereavement-program.
Every September, the Connecticut Hospice community of patient families, friends, and caregivers gathers to celebrate and remember loved ones who passed away during the previous twelve months. Connecticut Hospice understands the special importance of this year's event (honoring patients lost 8/1/19 - 7/31/20) as a safe opportunity to gather while also providing closure for families and friends who might not otherwise have had the chance during this challenging year.
Connecticut Hospice is proud to invite you to its first live, virtual event. This event is not just for Ct Hospice families but for all those struggling with loss. Please share this event with anyone you think may benefit. Simply click on link below to bring you to our YouTube channel.
Ceremony of Remembrance Sunday, September 13th at 4 pm via our YouTube channel:
This link will also be available on our website @ www.hospice.com and Facebook page at https://www.facebook.com/CTHospice
https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/stress-coping/grief-loss.html
https://www.psychologytoday.com/us/blog/supersurvivors/201909/the-power-rituals-heal-grief

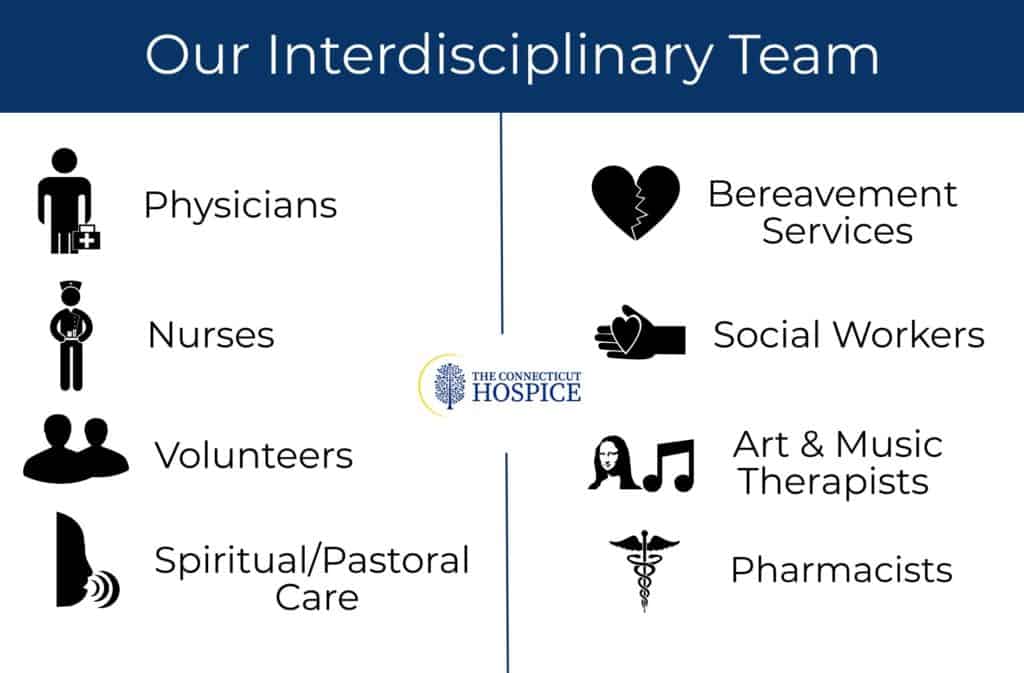
Caring for patients in a hospice setting is a nurturing and supportive effort that draws on the expertise of professionals engaged in many disciplines, ranging from medical to therapeutic. Indeed, the services offered by a leading hospice, such as The Connecticut Hospice, may in fact be broader and the care offered patients more varied than what is typically pictured by members of the public.
Even so, hospice-service providers remain concerned about the number of persons accessing hospice care late in the course of an illness. That’s per a new report issued by the National Hospice and Palliative Care Organization (NHPCO), which states that “53.8 percent of Medicare beneficiaries received hospice care for 30 days or less in 2018.”
More telling, is that fully a quarter (27.9 percent) of the beneficiaries received care for seven days or less— which NHPCO considers “too short a period for patients to fully benefit from the person-centered care available from hospice [providers].”
“This annual report provides a valuable snapshot of hospice care access and care, and also a reminder that we must continue to strive to make hospice care more equitable and accessible,” said Edo Banach, NHPCO president and CEO, in a statement. “It is also important to remember that behind these numbers are people who rely on person- and family-centered, interdisciplinary care to help them during a time of great need.”
Of compelling interest to hospice patients and their family members and friends are sections within the full 26-page report on what hospice care entails, how and where that care is delivered to patients, and what are the levels of care provided.
“Hospice focuses on caring, not curing,” NHPCO observes. “Considered the model for quality compassionate care for people facing a life-limiting illness, hospice provides expert medical care, pain management, and emotional and spiritual support expressly tailored to the patient’s needs and wishes. Support is provided to the patient’s family as well.”
The report also points out that, in most cases, “care is provided in the patient’s home but may also be provided in freestanding hospice facilities, hospitals, and nursing homes and other long-term care facilities. Hospice services are available to patients with any terminal illness or of any age, religion, or race.”
Indeed, the term “hospice” is somewhat elastic. It describes any approved provider of hospice services, including those that operate free-standing hospice inpatient hospitals and those that bring hospice care directly to patients where they are, be that a long-term care facility or in their own home.
The Connecticut Hospice (also known as CT Hospice) fits both descriptions, as it operates its own hospice hospital in Branford and fields teams of hospice medical professionals and caregivers to provide services at other caregiving facilities where patients are residing or right in the patients’ homes.
When hospice services are provided as in home, a family member typically serves as the primary caregiver and, when appropriate, helps make decisions for the terminally ill individual, notes NHPCO. “Members of the hospice staff make regular visits to assess the patient and provide additional care or other services. Hospice staff is on-call 24 hours a day, seven days a week. The hospice team develops a care plan that meets each patient’s individual needs for pain management and symptom control.”
An interdisciplinary hospice team usually consists of the patient’s personal physician, hospice physician, nurses, hospice aides, social workers, bereavement counselors, clergy or other spiritual counselors, trained volunteers, and speech, physical, and occupational therapists, if needed.
NHPCO lists these as interdisciplinary team services:
Nancy Peer, an Associate Professor for Hospice and Palliative Care at Central Connecticut State University, secured a bed for her son, Brian, who was dying of testicular cancer, so he could live out his last weeks at CT Hospice. “Every nurse that came in was not only compassionate… they would see how our son was doing and then they wanted to know how they could help us,” Peer recently told the Daily Nutmeg of New Haven.
Peer said that during the week Brian spent at the hospice, before dying at age 39 and leaving behind his wife of one year and his parents and a younger brother, friends and extended family were able to visit him and Peer and her daughter-in-law stayed with him. She remarked that the help he and his family received from CT Hospice was “priceless.”
The NHPCO report also details the four Levels of Care (as defined by the Medicare hospice benefit) that hospice patients may require. The levels are distinguished by the intensities of care provided relative to the course of a given patient’s disease.
“While hospice patients may be admitted at any level of care, changes in their status may require a change in their level of care,” NHPCO explains. “The Medicare Hospice Benefit affords patients four levels of care to meet their clinical needs: Routine Home Care, General Inpatient Care, Continuous Home Care, and Inpatient Respite Care.”
The report rightly credits the significant positive impact of hospice-care volunteers. “The U.S. hospice movement was founded by volunteers” and they “continues to play an important and valuable role in hospice care and operations.”
But volunteering is not a simple matter of stepping up to help others. The Connecticut Hospital, for example, requires that prospective volunteers receive a background check before coming onboard and then they are professionally trained by hospice staff to provide care and assistance to patients and their loved ones.
The importance of volunteers is underscored by NHPCO’s observation that “hospice is unique in that it is the only provider with Medicare Conditions of Participation requiring volunteers to provide at least 5% of total patient care hours.”
Volunteers typically provide service to others in these three general areas:

Spending time with patients and families (“direct support”)
Providing clerical and other services that support patient care and clinical services (“clinical support”)
Engaging in activities such as fundraising, outreach and education or serving on a board of directors (“general support”)
For information on volunteer opportunities with The Connecticut Hospice, please go to our website, www.hospice.com, or contact Joan Cullen at [email protected] or 203-315-7510.
The Connecticut Hospice is America's first hospice. It was founded by Florence Wald, and a group of nurses, doctors, and clergy, in 1974 and was the first of its kind in the United States. A few years prior, Wald, then an Associate Professor and Dean of the Mental Health and Psychiatric Nursing Program at Yale University, was inspired by a palliative care lecture given by Dr. Cicely Saunders, the founder of St. Christopher’s Hospice, the first hospice in the world.
Today, CT Hospice’s services encompass both in-home and inpatient care for persons diagnosed with a terminal illness with a limited prognosis, normally of six months or less.
The Connecticut Hospice’s central commitment is to enable the patient to live as fully and completely as possible during the time of their illness. This includes supporting the entire family as the unit of care, rather than just the patient. For example, home-care programs are designed to make it possible for families to keep the patient at home if such care is appropriate, and to marshal community resources to help deepen support and keep care costs as low as possible.

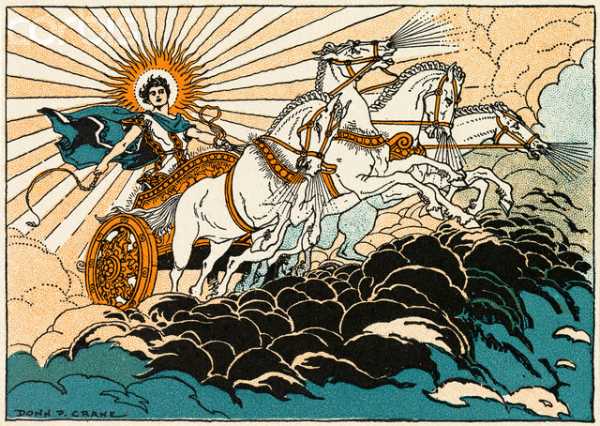
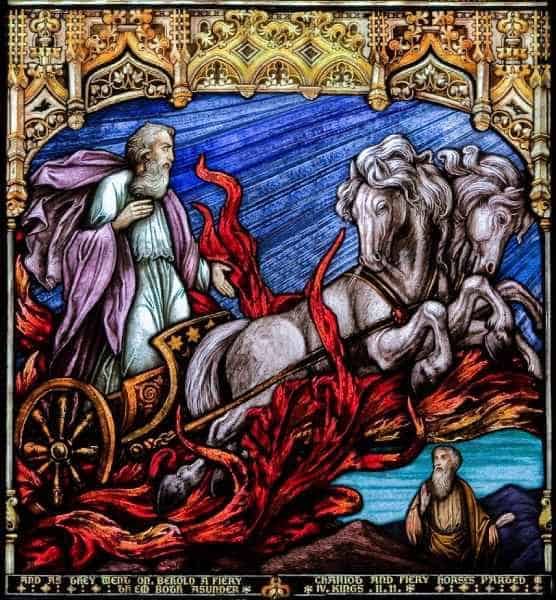
About an hour after my father died, I wandered away from my parents’ den, where he lay in a rented hospital bed, and went outside to be by myself for a while. On the horizon of the cold dusk sky the January sunset was a deep blazing red, more vivid than I remember seeing before or since. I imagined Dad shooting through the sky like a flaming arrow, for he was straight and true. Or like the Greek sun-god Helios arcing across the firmament in his chariot, for he was like the sun to me. Or Old Testament Prophet Elijah spiraling up to heaven in his fiery chariot, for Dad had (briefly) suffered, and deserved this final reward. Or all of these things at once.
These images were felt by me instinctively, and I didn’t share them with my mother, my sister or my daughter - partly because they were so intense I didn’t feel I could speak them aloud, and partly because a little internal voice said that I might be perceived as being melodramatic or even superstitious. Dad was an atheist, besides, and an academic family such as ours generally needed provenance, logic, or science to believe such things, surely?
It turned out that we needed none of those things, and a few hours later any doubts I had of such ideas were firmly swept away. Sitting in the dark on the family porch, I was startled by a lone goose, who flew down unusually close to the house, only honking when right in front of me, and then flapped away. It felt like a visit, and I went inside to tell my family about this “amazing phenomenon” before returning outside to the still night air.
About half an hour later Mum came to join me, and literally as she stepped through the door, a chevron of geese swooped down lower than any ever had before, all honking wildly as they flapped by. This had to be a sign, right? Lo and behold, when my sister came out to look for us another half hour later, yet one more goose suddenly appeared out of nowhere to make its presence known.

We all clung to the belief that this had to mean something, because believing the geese were visiting for a reason, that they might even be Dad saying goodbye, brought us comfort in that bleak “dark night of the soul”.
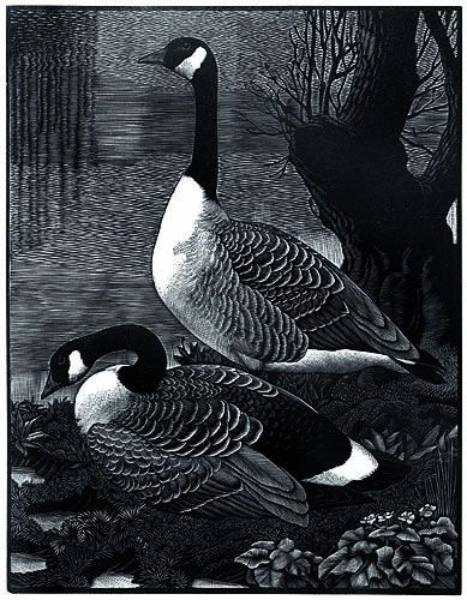
Since then, half the birds of the northern hemisphere’s skies have become ‘symbols of Dad’, such is our wish to remain connected to him in as many ways as possible. My sister and I have talked about this – she lives thousands of miles away, on another continent, and yet she sees the same ‘signs’.




For me, noble hawks always seem to circle overhead when I need his strength;
bright, persistent cardinals pop up in the nearby hedgerow when I want to chat to him;
mated-for-life swans scud silently by to remind me of his marriage proposal to my mother on the second day they met (married five weeks later, they were soul mates for 60 years);
never-shy catbirds hop right up close and train their beady eye on me in the same piercing way Dad always did;
squabbling blue jays even bring back family silliness, when we were a family together;
ephemeral, iridescent hummingbirds are rare and colorful visitors to my yard, but he was rare and colorful too.
And the seminally symbolic geese always bring me right back to the seismic shift in our world on that evening, when at one moment he was alive with us and in the next he had wrenched himself away.
Accepting and allowing that he was gone, in intensely painful slow motion, was like a long difficult labor, delivering a new reality.



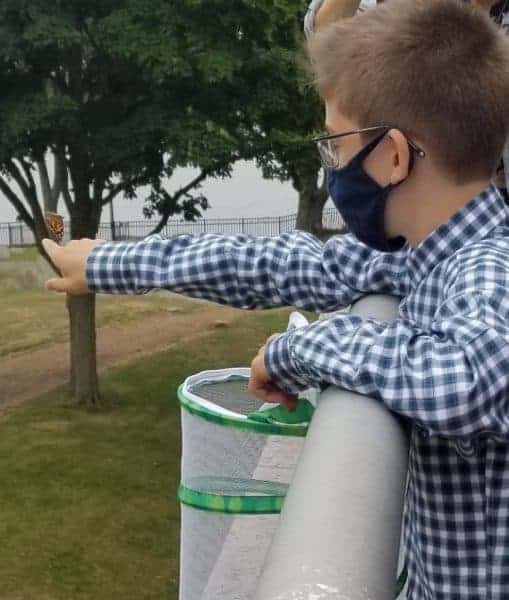
Why do human beings believe that signs and symbols from the natural world represent the presence of, or messages from, our loved ones after they are gone? For instance, many people believe that butterflies are deep and powerful representations of life. Butterflies are often thought to be a symbol of their departed loved ones or of eternal life, perhaps because of their metamorphosis from chrysalis to butterfly. Recently, Dmitri, a Connecticut Hospice staff member’s son, felt it was symbolic to release the 6 new butterflies from his Butterfly Garden on the site where hospice care first began in the United States.


Dragonflies are said to symbolize change and transformation, and are connected to signs from loved ones. Feathers, storms and rainbows are also often imbued with special meaning after a loss.




There are websites devoted to supporting the bereaved through the sharing of personal stories of ‘signs and symbols’ they have experienced. Click here for an example: signs of a deceased loved one
People often tell the recently bereaved to “look for signs – you’ll see them all around”, to reassure and comfort, and because they believe it to be true.
It seems that we try to hold onto someone we dearly miss by creating a physical manifestation where there is no longer a physical presence. That so many of these ‘messengers’ are animate entities of the natural world – animals, birds, insects, sometimes even flowers and trees – appears to bear this out.
It is well documented that nature has the power to bring solace and rejuvenation to us whether or not we are grieving, and it is plausible that we instinctively understand this capacity when we so readily ascribe special meaning to its creatures and its beauties.
Nick Cave writes
“The paradoxical effect of losing a loved one is that their sudden absence can become a feverish comment on that which remains. That which remains rises in time from the dark with a burning physicality — a luminous super-presence — as we acquaint ourselves with this new and different world. In loss things – both animate and inanimate – take on an added intensity and meaning”.
Nowadays, when Mum and I sit on the porch together, we sometimes talk about the ‘Great Creative Force” that connects all things. As an artist and woman of great wisdom, my mother can find symbolism and interconnection everywhere. Where once the anecdotes we heard about ‘signs’ from departed loved ones were possibly feasible, but mostly abstract, ideas, our family now knows and feels the truth of them.
We lost him but now he is everywhere.
Further resources:
To read Nick Cave's entire piece, click here: how to understand the experience of loss
To read an essay on birds and loss, visit: the birds scattering blue
What is the 'dark night of the soul'? To explore its interpretations, click here: the dark night of the soul - understanding amidst the absence of meaning
To hear the exquisitely beautiful "Dark Night of the Soul", Ola Gjeilo's composition for chamber choir, piano and string quartet (approx. 13 minutes), watch: Youtube: Dark Night of the Soul, Ola Gjeilo
Learn about and listen to catbird songs: All About Birds: Gray catbird sounds
All about Helios and how he is different from Apollo: Wikipedia: Helios
As a not-for-profit, we depend on generous donors to help us provide customized services and therapies that aren’t completely covered by Medicaid, Medicare, or private insurance.
Please make a gift to help us sustain the highest standard of care.
Admissions may be scheduled seven days a week.
Call our Centralized Intake Department: (203) 315-7540.