Please view our updated COVID-19 guidelines and visiting procedures →.

Dementia has several different forms, including Alzheimer’s disease, Lewy Body dementia, vascular dementia, frontotemporal dementia, Parkinson’s Disease-related dementia, and Chronic Traumatic Encephalopathy. All forms of the disease with the exception of Chronic Traumatic Encephalopathy, are terminal and last an average of seven to ten years, robbing people of their cognitive abilities, personality, and ability to care for themselves. Ultimately, people with dementia become bedbound and unable to talk, lose their appetites, stop eating, and become unrecognizable, emaciated versions of their once robust selves – devoid of the unique qualities that make each of us special.
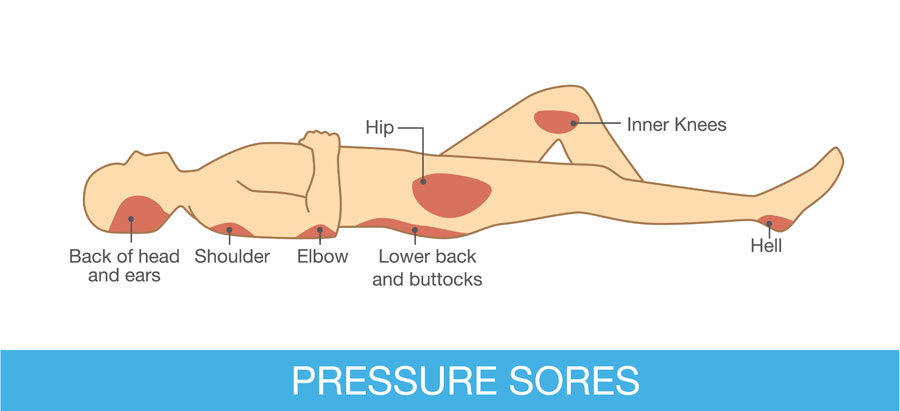
Complications such as difficulty eating and aspiration – inhaling food and fluid – with consequent pneumonia, and urinary tract infections and bedsores are very common. Other, later consequences of dementia, not necessarily seen in all people with this disease, are restlessness, agitation, combativeness, and inappropriate sexual behavior. Some dementias, such as Lewy Body dementia, are accompanied by hallucinations and delusions, including paranoia.
The management of dementia is time consuming, requiring dedication and patience as afflicted individuals become increasingly – and eventually completely -- dependent on caregivers for day-to-day activities such as eating, bathing, and dressing. Ongoing, high quality bedside care is essential to avoid – to the extent possible -- complications such as bedsores and aspiration. Failing to turn and reposition a bedbound elder for as little as five to ten hours can initiate a bedsore, which can rapidly progress to a deep, infected, ugly wound. Likewise, people with dementia should never be force fed – even so much as putting food in their mouths when they show no interest in eating – as this will almost guarantee their inhaling these oral contents into their lungs and getting pneumonia.
Reversal of cognitive injuries associated with dementia such as impaired memory and loss of executive function – like the ability to balance a checkbook or make a phone call -- is currently not possible; medications including oral cholinesterase inhibitors such as rivastigmine (Exelon) and donepezil (Aricept) and the new FDA-approved intravenous antibody therapies aducanumab (Aduhelm) and lecanemab (Leqembi) – administered every two to four weeks and costing $25,000 -- $30,000 per year – are used in early to moderate dementia to slow the progression of the disease and show varying efficacy – working better in some than others. The effects of these medications on everyday activities such as the ability to dress independently -- in contrast to delaying loss of memory and cognition -- are also variable, not possible to predict in any given individual, and may be minimal. Another concern is side effects; cholinesterase inhibitors commonly cause nausea, diarrhea, vomiting, decreased appetite, stomach upset, muscle cramps, fatigue, insomnia, dizziness, headache, and lack of energy, while the newer therapies may cause swelling and bleeding in the brain.
Several approaches may help to manage behavioral problems such as combativeness and agitation and should start with a search for underlying causes such as an infection or pain. Agitation caused by a medical condition is called delirium, which when treated may lead to resolution of the behavior and a far calmer loved one. Many elders with dementia have chronic painful conditions such as osteoarthritis or spinal stenosis and express their distress with restlessness and behaviors like repeatedly climbing out of bed instead of using words to describe their distress; this makes a trial of mild analgesics such as Tylenol a reasonable first step. Some may need more potent drugs such as opioids, as is seen commonly in hospice patients with dementia. Bedsores, for example, can be very painful. Urinary tract infections (UTIs) may also cause delirium, with the behavior resolving after a course of antibiotics. In the absence of obvious symptoms such as painful urination, flank pain, or fever, which may merit starting antibiotics immediately, however, investigation of UTI requires a urine culture to establish the diagnosis and avoid potential serious side effects of antibiotics such as severe allergy causing difficulty breathing or clostridium difficile diarrhea – “c diff” – which can be life threatening and easily spread to other, healthy people.
Other means of calming an agitated elder are environmental and behavioral, such as assuring a calm, quiet, familiar setting, soothing music, offering food when desired, turning out lights and turning down noise at night to allow sleep, and the presence of known loved ones. A chaotic, unfamiliar environment, with strangers randomly coming in and out of the room, absence of friends and family, constant light and noise, and painful procedures that interfere with sleep such as 5AM blood tests – done at this hour in hospitals to make results available for doctors’ morning rounds – may precipitate agitation, or make preexisting agitation worse. Hospitalization, often characterized by these negative environmental factors, can not only precipitate agitation, but accelerate the cognitive impairments and loss of ability for self-care that characterize dementia. Hospice staff hear again and again about elders with mild dementia who were still able to care for themselves before being hospitalized who were rendered bedbound and fully incapable of self-care after a one-week hospital stay. Sometimes, hospice staff are able to calm elderly people simply by seating them in a recliner at the nurse’s station and talking to them as they go about their business.

Underlying psychiatric illness such as depression, anxiety disorder, bipolar disorder, and psychosis such as schizophrenia may also trigger behavioral disturbances in demented elders, making treating these conditions – especially in people with preexisting diagnoses of psychiatric illness – another approach.
Finding an underlying cause of agitation is, unfortunately, the exception and not the rule in dementia, making the use of medications to try to treat delirium of unknown cause a reasonable next step. This, too, can prove difficult and is hit or miss. Numerous studies have been conducted to investigate which drug works best for which type of behavioral problem in which type of dementia, with mixed and limited findings. Drugs used include cholinesterase inhibitors, antidepressants including selective serotonin inhibitors such as escitalopram (Lexapro), sedatives such as trazodone (Desyrel) and lorazepam (Ativan), intended to improve sleep, anti-anxiety agents such as diazepam (Valium) and lorazepam, antiepileptics such as carbamazepine (Tegretol), and antipsychotics such as haloperidol (Haldol), risperidone (Risperdal), and quetiapine (Seroquel). It is always the goal of hospice staff to try to calm elders without sedating them so they can engage meaningfully with family and friends.
We treat pain and urinary infections where appropriate, establish a calm and soothing environment, assign staff and volunteers to sit at the bedside to talk and read to patients, have members of our arts department play live music for them, seat them collegially at the nurse’s station, try to assure their sleep with moderate doses of sedatives at night in a dark, quiet room, and allow their loved ones to visit 24-7. If these interventions don’t work, we use antipsychotics and other medications that are less sedating and do not escalate to higher doses of sedating agents until all other interventions have been tried and exhausted. At times, rendering someone sleepy or unconscious may be the only way to relieve agitated delirium, a symptom that may be as distressing for our patients and their loved ones as severe pain or shortness of breath.
In all cases, our goal is to maintain the dignity and humanity of all of our patients to the extent that is humanly – and medically – possible.


As a not-for-profit, we depend on generous donors to help us provide customized services and therapies that aren’t completely covered by Medicaid, Medicare, or private insurance.
Please make a gift to help us sustain the highest standard of care.
Admissions may be scheduled seven days a week.
Call our Centralized Intake Department: (203) 315-7540.