Please view our updated COVID-19 guidelines and visiting procedures →.

The Connecticut Hospice, established in 1974 as the first Hospice in America, has always been dedicated to honoring all patients and families affected by life-limiting illnesses with integrity, support, and compassion. This dedication includes an increased commitment to the special needs of veteran patients and is supported by a new partnership with the We Honor Veterans program.
We Honor Veterans is a collaborative effort by the National Hospice and Palliative Care Organization (NHPCO) and the Department of Veterans Affairs (VA), which invites hospices and VA facilities to join a program focused on serving the unique needs of America’s Veterans and their families. Participating organizations bolster their service to Veterans by moving through five levels of partnership.
At Connecticut Hospice, the We Honor Veterans program is viewed as a great opportunity to formalize and advance the organization’s commitment to veteran patients. As We Honor Veterans has become more integrated into the organization’s services offered, the positive impact on veteran patients and their families has become evident from the smiles on the patients’ faces.

The most recent veteran-focused event was held this past Memorial Day, May 30, 2022, when Connecticut Hospice welcomed Branford, Connecticut’s Scouting Troop # 688, representing the Boy Scouts of America, to present the colors at a special honor guard ceremony.

Some Connecticut Hospice patients, families, and staff assembled on the waterfront side of the campus to partake in the event, while others watched from their room windows. The scouts, ranging in age and rank, were accompanied by troop leaders, Michael Loffredo, Brian Appleby, Deidre Salemme, and Crystal Bailey-Loffredo.
The Memorial Day program opened with a prayer and a brief history of Memorial Day. Scout Master Loffredo then read the legendary Gettysburg Address, which President Lincoln delivered on November 19, 1863. Scout Master Loffredo also gave a detailed account of wars with American involvement, including years fought and the number of United States servicemen and women who have lost their lives – currently this is quoted at over 1 million. The afternoon concluded with the playing of Taps by a member of the troop, a recitation of the call’s lyrics, and finally with the retiring of the colors.
Both the scouts and troop leaders took the opportunity to interact with several of Connecticut Hospice veteran patients, who proudly attended the special Memorial Day presentation, and thoroughly enjoyed sharing his military stories to an eager audience.


Prior to the day’s events, our Veteran Volunteer, Joe Marino, who served in the army as a dentist in both Desert Storm and Gulf War, presented personalized recognition certificates to all Veterans currently receiving care in our inpatient hospice unit.


Connecticut Hospice has also implemented a process of placing a small flag on the bottom of a veteran patient’s bed upon passing. It is just another way to pay respect to veterans for their service.
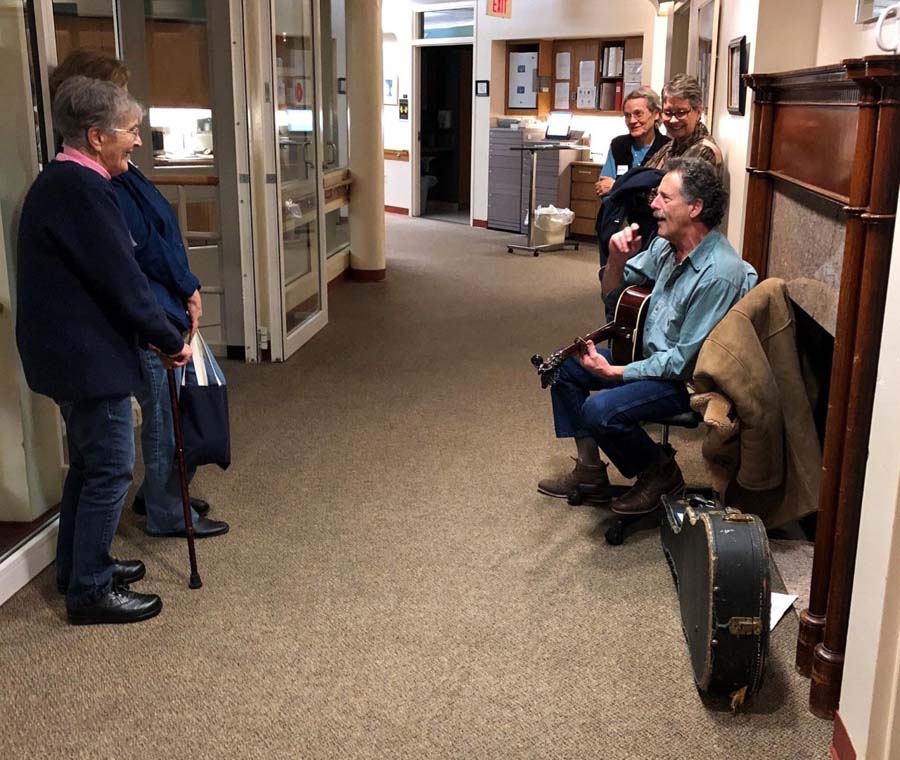
The arts enrich everyone’s days, and they are equally important at the end of life. At The Connecticut Hospice, we live out this philosophy. We employ music and art therapists to work with patients and families, both in our facility and in homecare settings, and use dozens of volunteers to fill our halls with art and the sound of music.
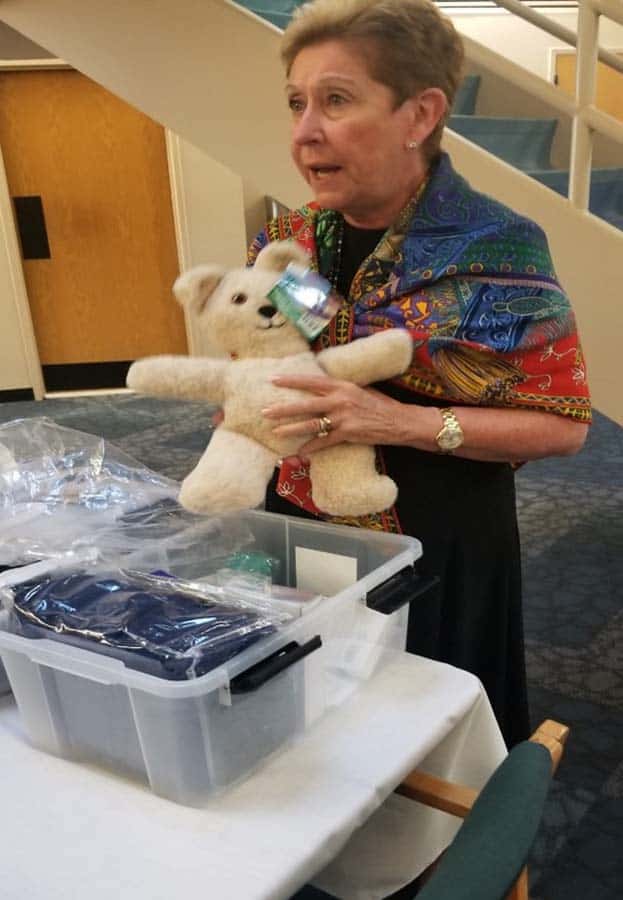
We also keep a large library of CDs and CD players that can be borrowed by patients and families to be played at bedsides, and we hear everything from opera to jazz to Disney songs, as people connect and reconnect through the music of their past lives. For our patients diagnosed with dementia, music is so important that we have tiny MP3 players embedded in teddy bears, which have been programmed to play music chosen by families to evoke positive thoughts and feelings. Often, it comes from an era long ago, and taps into old memories.
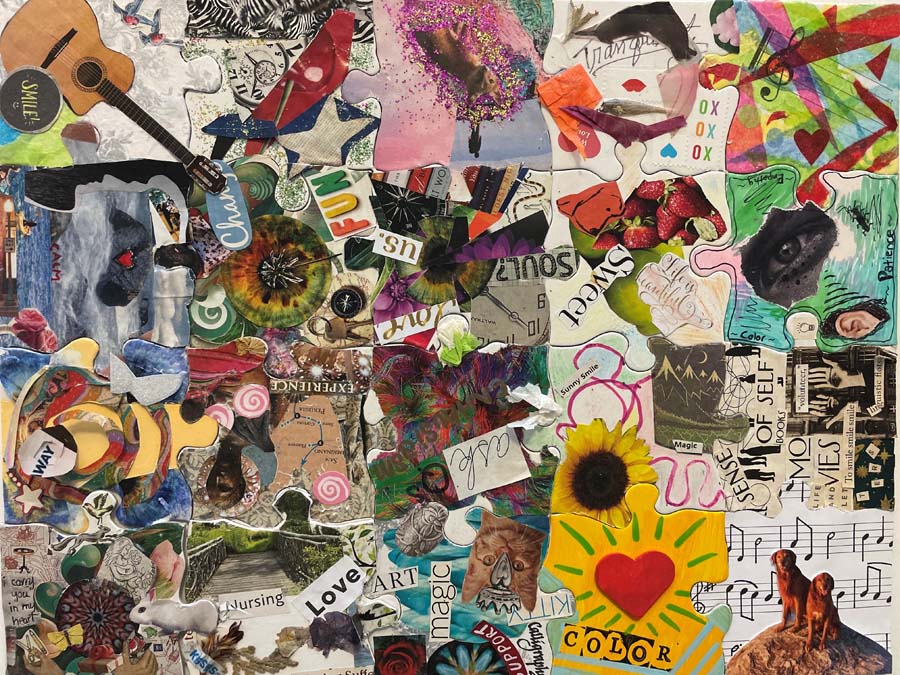
That technique begins to touch on art therapy, which is different from performing on an instrument or drawing in front of a patient. Art therapists are specially trained to use their talents to help patients and families process emotions, fears, and need for closure. They work with patients to create memorials to leave behind. One patient used our help to make videos for the next birthdays of each of her loved ones. Another patient worked with our art therapist to illustrate the lyrics of a song she wrote with our music therapist, which was then recorded and given to the family as a gift. Some make physical tokens of their love, or collages displaying life memories.

Children especially flock to our arts staff to work on pieces that often show what they cannot express directly. They may be frightened or confused, and just the process of sitting down to make something can both calm and direct them. In addition, it gives space for other members of a family to have conversations in which they are not involved.
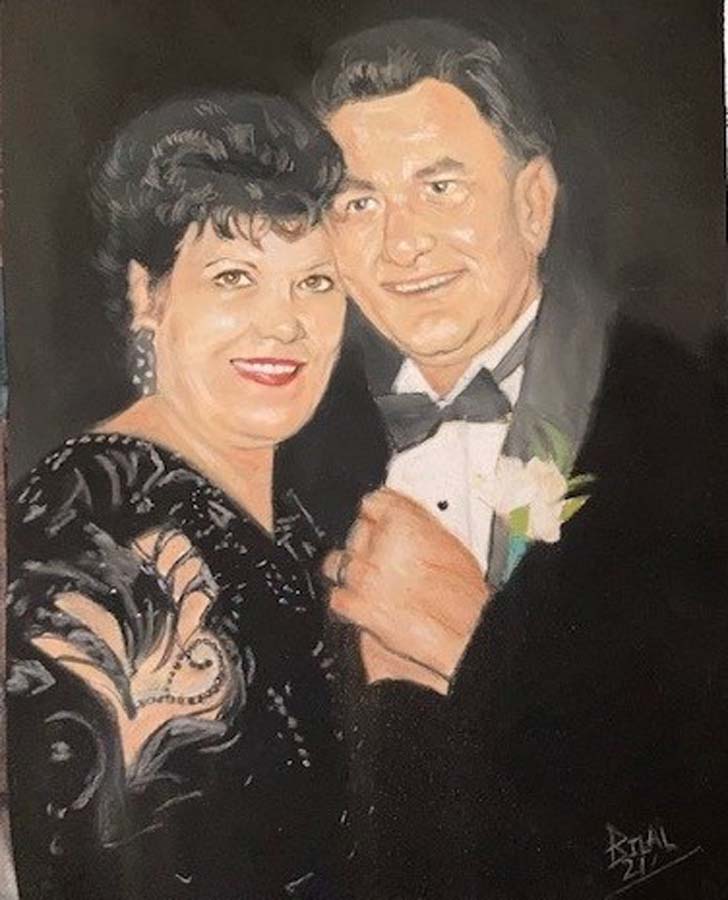
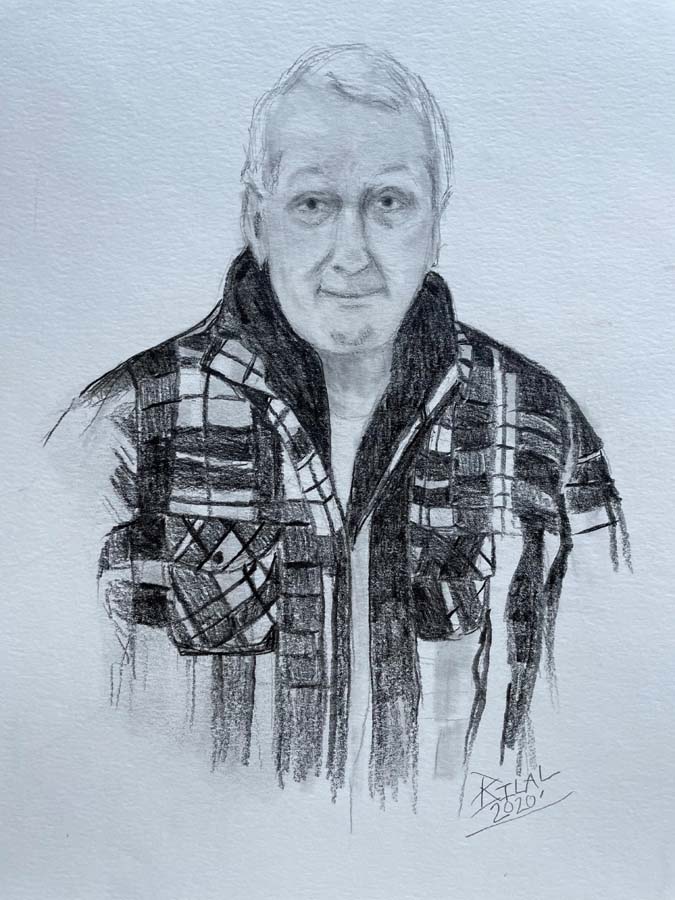
One staff artist specializes in portraits. She draws people from a photograph provided by the patient or their loved one. Families then have that drawing to keep, and often display them at celebrations of life or other ceremonies.

For staff members, being surrounded by art and music makes a difficult job easier. We all know that music and art are soothing, and we all take advantage of its presence to slow our breathing or change our moods. Many of our volunteers who play, either on our lobby piano, or in the wings of the patient floor, are longtime regulars, and we look forward to their “shifts”, when we can enjoy our favorite selections—sometimes by request. Occasionally, several families will connect over an impromptu concert, and even stand around the musician, singing together. At Christmastime, carols are a must for many.
- by Hannah Righter, Connecticut Hospice Director of Arts
(For this story, we’re going to call the patient Joe and his wife Sally.)

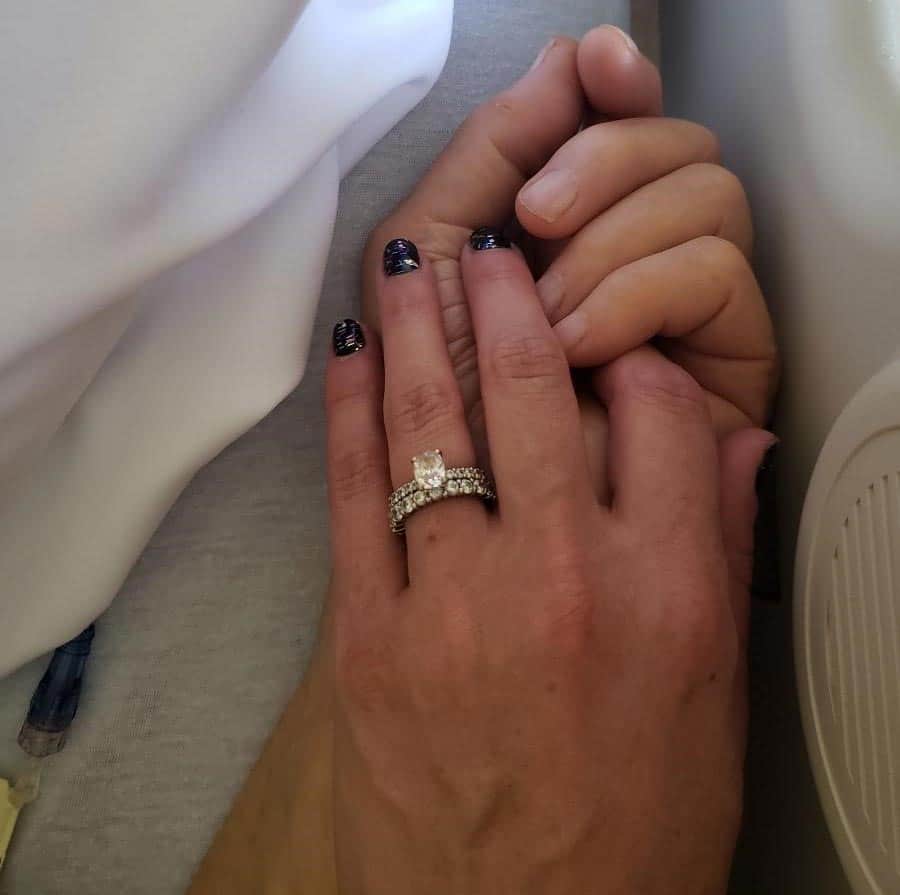
Both Joe and Sally had remarked on the soothing, cathartic, and memory evoking benefits of music during previous sessions, though what occurred during this visit was truly spectacular.
In this session, Joe was lying in his hospital bed with Sally sitting beside him. Both welcomed me into the room with a warm smile and shake of the hand. The session began with a song that I learned per the wife’s request prior to this visit. During the song, Sally held Joe’s hand and softly sang along. Once the song was over, Joe began sharing memories of his travels throughout the years, which then made Sally think of another song, which I played on my guitar and sang. Joe then smiled while vividly describing Rome, Italy, sharing that of all his travels, this location was a favorite of his and his wife’s. Joe then stated “you're not just bringing back memories, you're bringing back a picture. I can actually see it.” Now, what made this statement exceptionally significant, is that Joe had lost his vision and was legally blind at that time. Joe then went on to laugh and smile while recounting fond memories of this trip, one more vivid than the next. The session continued with more patient preferred music, laughter, storytelling, and singing along. At the end of this visit, Sally walked me to the door and while expressing gratitude, stated “whenever I tell him you're coming he really perks up.”
This visit details the ability patient preferred music has on evoking memories and bringing patients and their loved ones back to a very special time and place in their lives. This act of reminiscing can be just as meaningful and cathartic for families, especially when their loved ones (patients) are at a point in which they can no longer communicate verbally. It provides the opportunity for them to share stories beyond symptom and diagnosis. This helps paint the picture of important aspects throughout their loved one’s life and allows us to get to know (and treat) them as a whole.
Also, because of this strong emotional connection between music and memories, patients who may not be able to speak coherent sentences can sing along to songs they enjoyed listening to in their younger years. We see this type of engagement (maintaining eye contact, tapping to the beat, singing along) quite frequently and is just as beneficial to our patients as their loved ones who are able to share these meaningful interactions through music.
- by Hannah Righter, Connecticut Hospice Director of Arts
(For this story, we’ll be referring to the patient as Maggie.)
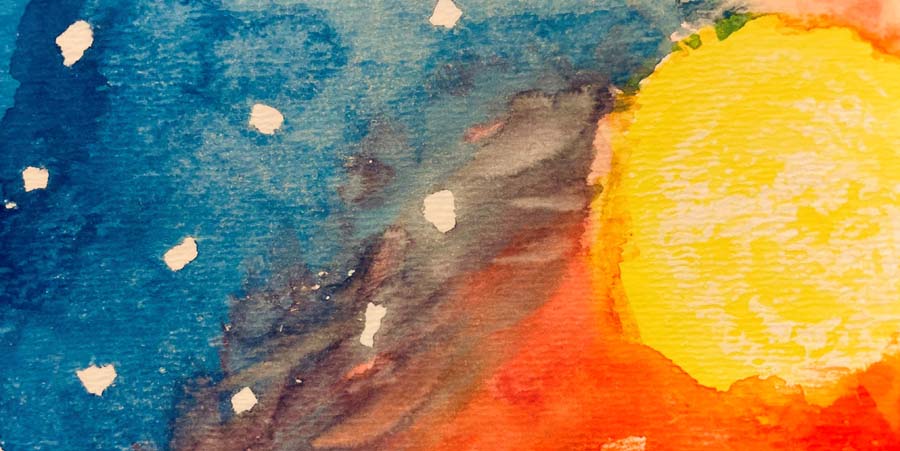
Maggie was having a particularly difficult day and had been referred to music therapy to provide emotional support and help decrease some of the anxiety she was experiencing at the time. When offered music, Maggie initially declined, requesting “sit with me and talk.” After some rapport building conversation, Maggie expressed desire to create artwork with the theme of "wind on a stormy night," stating that to her, this acts as a reminder that "even when it's stormy, we have a place that is safe [CT Hospice] and we have each other." Maggie actively participated in the art making process through placing tape on the paper to indicate where the stars would go, directing where to start and stop the swirls that represent the wind, and selecting the colors to use. Throughout the session, Maggie held her hands to her chest, made positive remarks, and laughed and smiled while exclaiming "I'm an artist!"
Maggie reminisced about time spent with friends and family and shared her belief that everyone should be treated, respected, and loved equally. At the end of this visit, Maggie spoke again about the theme of support that she felt was represented by the painting. Maggie then held my hand while stating "we have each other." Maggie went on to express the profound support she has received while at Hospice and how comfortable she felt following this session.
This session is a prime example of using art and music (painting in this case) to support the conversation and need(s) in that moment… to create an environment in which this individual felt safe and comfortable expressing herself, and essentially use the arts to address clinical, non-arts related goals (self-expression, coping, emotional support).
Sometimes there are not words to express exact feelings, especially in this setting, though there is a song that resonates or artwork that can be created. In this case, the patient was experiencing increased anxiety and was able to use the arts to express her feelings in a creative and non-threatening way, process her emotions, and create a piece of artwork that represented her own resilience and support system.
There are so many anecdotes like these two, and they all illustrate the importance of the arts in meeting the needs of patients and families in innovative ways. The last such story involves a patient with advanced dementia, who no longer spoke or responded to anyone. His wife requested what she referred to as “their song”, and the music therapist played that for them by his bed. He opened his eyes, and said “Shall we dance?”. We then discovered that the couple had been competitive ballroom dancers many years ago, and that the song was the one they used in competitions. Such is the power of music to evoke memories, and, in this case, abilities!
The arts represent just one of the ways in which hospice care can reach people at the end of life, helping them find peace and closure. Although we have skilled professionals who do this on a daily basis, music and art are tools that everyone can use in such situations, and bring smiles through the tears.

One of the members of the Hospice team is a chaplain who interacts with other team members in providing total care to our patients who are facing end-of-life issues. In the context of hospice care, spiritual issues and/or spirituality is not confined to one singular religious experience. The chaplain has a broad knowledge of many world religions and is sensitive to their understanding of how these challenges intermesh with the patient’s faith journey at this point in time.
Spirituality may not include an organized faith journey for some of our hospice patients. A sense of meaning in their place in the world in relation to nature, humanity, and a sense purpose all come together in a form of recognized spirituality. The Connecticut Hospice chaplain is here to listen and accompany the patient through this journey.

Spiritual Care is an important component of the comprehensive care plans at Connecticut Hospice. The Hospice Chaplain sits and listens firstly to the patient and hears what they perceive as what is occurring to them. They may express fear, have an unknown feeling of uneasiness, or lack acceptance of the concept of end of life. The chaplain hears the many concerns and transforms these issues into a plan of care. This plan is utilized to help the patient address their issues and to be comforted in the end-of-life process. As chaplain and patient progress in their relationship, adjustments may be made to further a compassionate plan of care that is individually designed to each person’s perceived needs.
This process includes family and friends who can give insight that the patient, because of illness, is not able to remember. The chaplain is also present for family members who struggle at this time of perceived loss. There are so many emotions present: anticipatory grief, anger, depression, and guilt. They begin to manifest themselves in many diverse ways. The chaplain, who is a trained medical-spiritual professional, can address these issues as they arise in the patient and with family members. The Chaplain, as a member of a highly trained team, receives observations from the social worker, nurse, doctor, and team directors that prompts changes to the plan of care to be sensitive to comfort and compassionate care.
A healthy spiritual outlook connects to an overall sense of well-being. This can affect the management of pain, producing a higher level of mental physical comfort. The main hospice goal is always comfort. The chaplain aids in accomplishing that objective.

Chaplains understand the intimate relationship patients have with religion, spirituality and the nature of earthly existence and, specifically, different ethnic cultures. They have spent many hours studying cultures and how they affect each and every being. Even though the family and patient may heavily rely on local clergy, the chaplain is critical in providing ongoing presence and developing a friendship that brings comfort and assurance to all concerned. When the family has its own clergy or spiritual guide, the Hospice Chaplain can assist in notifying that person, and arranging a visit. This specific attention from a pastor is different from the broad spectrum of what spiritual care can encompass.
Looking once again at families, as time progresses and their loved one’s illness progresses, new emotions and expressions among family members emerge. A weekly call from the chaplain can be very beneficial to the family, just knowing someone else cares, someone else understands, someone else knows how they feel.
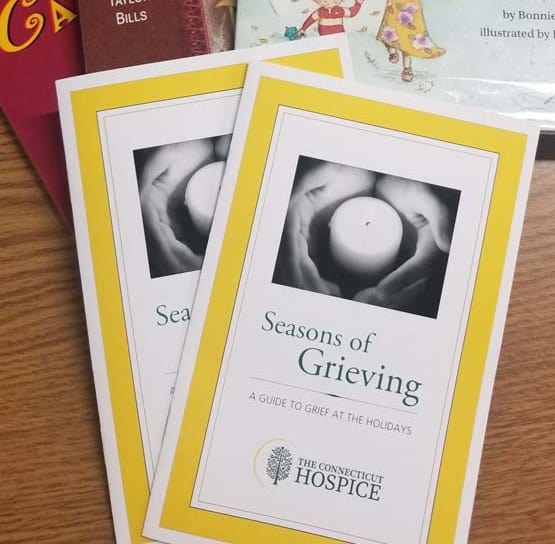
The Chaplain may suggest reading material that can guide them in their emotions. Sometimes there is a specialized plan for children in what maybe a first-time experience with end-of-life issues. The chaplain is prepared to gently explain what is happening to grandma and to compassionately listen to and answer their questions.
As time progresses, we continue to honor the hospice philosophy that no one should approach death alone. As a critical part of the team, the chaplain is present, if applicable, to once again inform the local clergy, if desired by the patient or family. He or she will be invited to join in with the team in aiding the patient to transition comfortably. The Chaplain, who has at this point developed a relationship with the family, has become a trusted member of the patient’s circle. The chaplain knows the patient’s needs and can help by expressing them at this crucial moment. Again, no one dies alone. Family members will be called and informed that death is near and the chaplain will be present as a guide.

Family members may need counseling or compassionate listening at this time. The chaplain can find a neutral place to allow family members to express their feelings and needs. When death occurs, the family can gather with the chaplain for prayer and blessing.
The journey can continue with the family with helping in appropriate funeral planning in keeping with cultural, religious, and spiritual understanding of each unique family situation. In the weeks ahead the chaplain and a specialized bereavement team member will check in with the family.
Sometimes we are asked to give prayers, or even facilitate a service for the family and friends of the loved one. Then, along with the social workers, we usually turn to the Bereavement Director, who steps in after death, for the thirteen months of grief counselling formally provided. While time limits are fluid, the year or so of formal groups or sessions is seen as a benchmark by Medicare, that accommodates most survivors in that setting.

Currently, Connecticut Hospice has a team of three pastoral care professionals, along with six social workers and a Bereavement Director. In addition, we have many volunteers, who participate from the time of admission, through the transition itself—especially when family members are not able to be present—and afterward, to assist in many ways. Many of them have suffered similar losses, and this is their way of giving back what hospice care provided to them in their time of need. Every team member offers a unique and highly specialized view towards hospice care. The chaplain is one of the team that aids all concerned to a compassionate, informed journey through the end of life.


Many people know that hospice care benefits are mandated by Medicare such as skilled nursing, aides, durable medical equipment, drugs, and ambulance transportation, among other things. What fewer realize is that those benefits extend to the survivors, in the form of bereavement support for 13 months following the death of the patient. It is rare for a program to include services to others, and many who do not take advantage of a bereavement program may not even know that it exists.
At the Connecticut Hospice, bereavement care is a part of the Social Work department. That group handles intake assessments, including bereavement risk, at the time of enrollment. Clinical skills and long experience enable social workers to evaluate the patient’s family, in order to try to determine whether there are those who might be at risk of not coping with the death of the patient. There are attempts made at that point to try and provide support and counseling, which includes bringing in the Spiritual Care group to assist wherever possible.
The IDT (interdisciplinary team), which meets every other week and evaluates the care needed by each patient and family, is enlisted in a general discussion of psychological as well as physical needs. Everyone who deals with the patient and family is encouraged to note problems or issues, and to enlist the aid of others on the team in helping to address them.
As a patient nears the end of life, Social Work offers help in planning for arrangements after death, and with the expected anticipatory grief. After a patient passes on, the caregivers involved with that family usually reach out and express condolences. At that point, the Bereavement team generally takes over. This process can take some time, and it is not uncommon for people not even to remember being called, or offered bereavement services. That’s why they are contacted at other, later, times, when help may be more readily accepted, both by phone and by letter or card. Many people describe those early days as being in a state of numbness, often accompanied by overwhelming exhaustion from weeks or even years of caretaking. Bereavement at that immediate time is separate from the processing that takes place over the months ahead.
Some surviving family members request individual help, with specific chores, or with more general emotional issues. If it is appropriate, some will also be referred to outside therapists or psychiatrists, for more intensive treatment. Others take advantage of grief groups, which can be specifically for particular people, such as spouses, parents, or children. Some groups are run for one gender only, to increase the commonality of concerns and feelings. At Connecticut Hospice, we open our groups to members of the broader community, including those who were not enrolled in services provided by us.
Most groups last for a few months, although it is common for at least some members of the group to remain in contact with each other in an informal way going forward. Sometimes, the seasons dictate the agenda, as when people face holidays, and the need to take over certain functions or to create new traditions. One participant stated that her friends and family were supportive, but that it was invaluable to be in conversation with others who had gone through the death of a parent, just as she had.
Many family members choose to stay involved with Connecticut Hospice, and some of our best volunteers come from the ranks of our bereavement groups. Our policy is to have people wait a year before becoming a volunteer, since raw grief is not always helped by constant contact with other grieving families. However, once that time has passed, it can be very soothing, and provide great closure, to be able to pay it forward to others.

Everyone at Connecticut Hospice deals with grief on a daily basis. They understand the forms that displaced grief can take, and they are almost unfailingly patient and kind, even in the face of unbridled criticism. It’s a delicate balance to be warm enough to help a person cope by providing sympathy and compassion, but to be emotionally tough enough to take the lashing outs that can accompany the grieving of others. In fact, our social workers do some of their work with the clinical staff, addressing those situations and helping us to process them appropriately.
Once a year, we have a Service of Remembrance for everyone who has died in our care in the prior year. It used to take place with hundreds of relatives and staff in a giant tent. Since COVID, it is online, with both taped and live-streamed portions, and is accessible throughout the year to families and friends. It is impossible not to tear up as the names and faces of each of the patients scroll across the screen.

At the end of the service, music wafts through the air, as flowers representing those who have passed are carried in baskets down to a boat on the shore (In fact, the service time is changed each year, in deference to the tides). The boat slowly makes its way out to sea, and the flowers are dropped into the water, where they float as a lovely tribute.

Grief follows its own timetable, however, and everyone recovers in his or her individual way. Connecticut Hospice continues to serve as a resource, with written materials, online articles, and opportunities for the families we have served to engage with us in our mission. We consider it a privilege to aid loved ones through the end-of-life journeys of our patients. We don’t forget them. We learn from them, celebrate their accomplishments, retell their jokes, recount our memories of them, and think of them when we gaze out on beautiful sunrises and sunsets over the water, which evoke so well the circle of life we all share.

“Palliative Care is specialized medical care for people with serious illness, focused on providing relief from the symptoms and stress of the illness. The goal is to improve quality of life for the patient and the family. Palliative care is an essential part of the care of anyone with a serious illness, including people who are continuing to be actively treated, and can not only help people get relief from symptoms like pain and shortness of breath, but also help them to better understand their illness and its treatment so they can choose the care that is right for them -- from ongoing active treatment to hospice.
Palliative care is different from hospice care because it is appropriate for people who are seriously ill and are continuing treatment. With exceptions, such as continuing routine medications for problems like high blood pressure or diabetes, people in hospice care are no longer being treated for serious or terminal illness. For example, people in hospice care are not treated with chemotherapy or radiation for cancer, and focus instead on the relief of symptoms.”
Joseph Sacco, Chief Medical Officer, The Connecticut Hospice

The terms “palliative care” and “hospice” are often used interchangeably, confusing patients and families alike. Many hospitals now offer palliative care services to those in pain. Some are in hospice care as well, some are having active treatment for their diseases, and some are only receiving palliative care for pain management.
Those of us in the field are often guilty of this confusion as well. Often, people who are resistant to the term “hospice”, but are past the point of curative care, are referred for palliative care instead, either to a home health agency or to a home hospice agency.
We have traditionally provided both palliative and hospices of care at the Connecticut Hospice, but have found that, almost without exception, the level of services is fairly comparable. For this reason, we have begun limiting the intake of palliative care patients, as we are judged by CMS, (Centers for Medicare & Medicaid Services) by their level of functional improvement.
Since many are at or near the end of life, little progress in the tasks of daily living is achieved, causing us to get very few stars in the government’s rating system. Hence our hesitancy in taking on patients with whom we cannot succeed, by the Federal definition, yet who truly need our help and care. This is a problem that needs addressing, both by the Federal government, and by physicians. Busy doctors are more likely to suggest palliative care, because it doesn’t carry the weighted overtones of “hospice”.

All of this overlap really goes back to the original Medicare definition of hospice eligibility, which was apparently set more or less randomly at six months of life expectancy at the normal disease trajectory. While that may mean very little in the case of an individual, it has become a catchphrase for our industry, depriving those who cannot be certified of important services, and deterring others who are loath to accept an arbitrary six-month prognosis.
Those of us in the hospice line of business believe that it’s past time to change that standard since the evidence is clear that many, if not most, hospice patients have their lives extended with the skilled and compassionate care that hospice workers give. In addition, people in the care of home hospice are frequently able to avoid or minimize time spent in hospitals and urgent care settings, which patients find very taxing and debilitating, without even considering the expense of multiple hospitalizations. If the time frame being discussed were twelve or eighteen months, more patients would likely choose home hospice, and possibly live as long or longer than with aggressive treatment.

The issue of continuing treatment is complicated and also seems to be transitioning. There are many patients who continue to seek treatment for their disease because they can, and, even if it’s a long shot, they don’t want to stop. Since hospice care is considered to be CMO (comfort measures only), and since hospices are required to pay for all treatment and equipment related to the patient’s diagnosis under hospice care rules, this means that we can’t afford to take someone who is undergoing treatment.
Palliative care is compensated at a much lower rate, meaning that caring for a very ill patient continuing treatment, but needing end of life care, doesn’t make financial sense for a home care agency, if that means that they are providing hospice level care, but being paid for routine palliative care. A terminal patient still having treatment is just as sick, or sicker than, a patient receiving comfort measures only, yet the payment for palliative care is far less than for hospice care. In the case of hospice care, even if an exception is made for certain types of treatment, the expense of that treatment puts it out of reach for hospice budgets.
When deciding on care for a loved one, all of these factors can come into play. It’s hard to discontinue treatment from an emotional point of view, even if it is causing side effects (although newer infusion therapies and immunotherapies are much more likely to be tolerated easily). Also, doctors are taught to cure, not to counsel acceptance of death. However, many patients live fuller, and even longer, lives when symptoms are managed and care is compassionate but not meant to be curative.
This is where the confusion of terms comes in: We would consider that symptom management is both hospice care and palliative care. From a home care billing point of view, however, the two are separate, with palliative care used to mean care for a serious illness where improvement is expected, and hospice care used to mean care for the same illness, once the goal of curing the disease has been foregone. To confuse matters further, Palliative care in hospitals can be “comfort measures only”, which is technically hospice care, or pain management. It’s no wonder that families get confused!
The most important starting point is for the patient and his/her support team to have an honest conversation among themselves, and with their treating physicians, about the effectiveness of current and future treatment, a true prognosis for the disease at hand, and the goals for that person’s life trajectory. Some will choose length of life, some will choose quality of life. Sadly, it often happens that assumptions are made, or hard truths are not voiced, so that treatment and care can be working at cross purposes.

If treatment is still desired, a hospitalized patient may still see a palliative care doctor, but the medical team’s efforts are aimed at gaining a cure, or a remission, of the illness. In many cases, this aim means that the patient may have more discomfort, both from the disease and from the treatment. Doctors also can’t know for sure how different people will be able to tolerate, or not, various regimens for treatment. Often, it is not clear early on whether treatment will work, so all of these factors need to be revisited regularly.
When a patient and his/her family come to the decision that comfort care is the way to go, our full attention can be mobilized in that direction. After decades of experience, we have become experts in delivering care whose aim is to fulfill wishes, promote comfort and closure, and relieve pain. Since our goals are less long term, tolerable pain levels are often left to the patient; he/she might choose to remain more lucid, albeit with discomfort, or to be more sedated and have more relief.
It should be clear by now that the patient and family are at the center of this choice, as they should be. All people should be given enough information to make the decisions that are in their own best interests. In fact, that was a primary reason for our founder, Florence Wald, to establish The Connecticut Hospice as the country’s first hospice. She believed passionately that patients and their families needed to be considered as a unit, and that they should be given their diagnoses and prognoses, which wasn’t commonly done fifty years ago. She trusted in the innate wisdom of those at the end of their lives to decide how to spend their remaining days, months, or years, and in the ability of nurses and other medical professionals to help those wishes to come true. And that is as true today at The Connecticut Hospice as it was at our inception.



Having seen tens of thousands of patients over the past five decades, The Connecticut Hospice has the highest amount of professional skills for end-of-life care management. Over time, The Connecticut Hospice has progressed from its original beginnings—providing care for cancer patients and their families—into serving all patients, regardless of diagnosis. One of the conditions which has seen a huge increase in incidence is dementia, in part because other diseases can be cured or controlled, leaving more people to suffer from mental decline at the end of life. This can be particularly hard on families, who are often grieving the loss of the person they knew, while that loved one is still alive. Our new program, Magnolia Care, will increase the services and support to patients and families with Alzheimer’s disease, and other cognitive failures.
The training that we are giving to our nurses, aides, and social workers, combined with our longstanding knowledge of treatment options that preserve quality of life, has allowed us to design Magnolia Care in the most thoughtful of ways. In order to best understand what we are offering, it will help to provide some explanation of the progression of dementia.


Between 5 and 8% of the U.S. population over 65 is living with some form of dementia, with that number rising to 50% of those over 85. Dementia is defined as cognitive changes that affect thinking, personality, and behavior. It can be difficult to diagnose in its earlier stages and can be confused with other causes of those same symptoms. However, it occurs broadly across these age groups and is expected to increase as life expectancy rises and more people enter this demographic.
Early phases of the disease can often be managed by families without outside support. Minor adjustments in daily living arrangements, or additive monitoring of complex tasks, can suffice for some period of time. Independent living may be a challenge but is sometimes prolonged with enough support from relatives or paid caregivers.
The final stage of most diseases of dementia occurs between 3 and 6 years after a diagnosis is made. The progression of the disease does not follow a specific timeline and is different in each case.
This period of advanced symptoms may be months or years in length and could include a variable course of events which is unpredictable. Regardless of the type of dementia, there are some typical features that are often common at this time:
Magnolia Care is designed specifically for persons living with dementia at the end of life. Nurses, social workers, chaplains, nurse aides, art and music therapists, and volunteers all undergo intensive training and are certified in person-centered dementia care and non-pharmacological interventions.
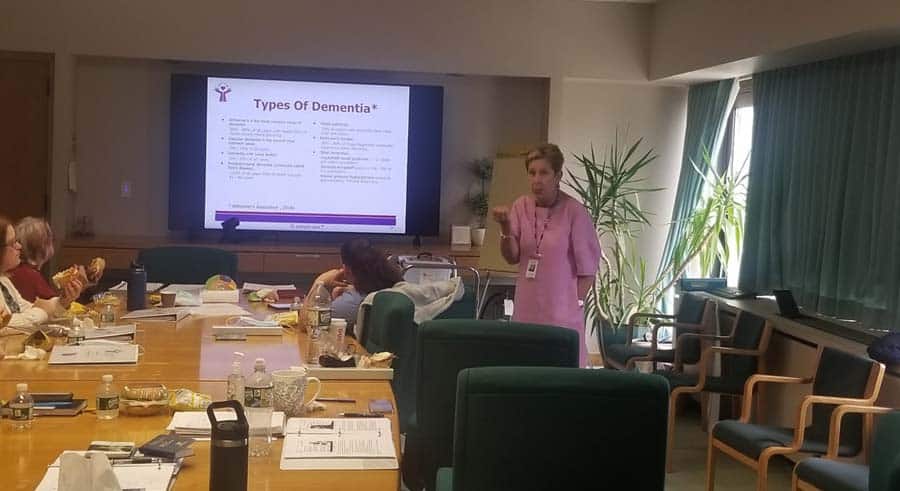
Our final-stage dementia care training was created by a hospice nurse with extensive experience caring for patients with dementia. This dementia-expert-lead training focuses on the behaviors and needs of hospice patients with cognitive failure, ensuring that Connecticut Hospice caregivers can recognize and respond to the concerns of dementia patients and families.
Like all of our Hospice Care programs, Magnolia Care provides a comprehensive approach that incorporates all the members of the hospice team in a plan of care that addresses the unique needs of each patient.
We have assembled a “tool kit” for use in homes, nursing homes, or assisted living, which offers enhanced tools for the management of symptoms, and can allow patients to access deeper memories, providing both solace and joy. The goals are to reach those patients where they are in their journey, help families to communicate and comfort their loved ones, and reduce the need for pharmacological solutions to common problems with behaviors.
Music is a known soother of dementia symptoms, and we work with caregivers to provide appropriate and significant music, tailored to the individual’s taste and age. MP3 players are embedded with this music in teddy bears, comfortably used by even people who are cognitively impaired.

The toolkits also include a diverse range of items to help dementia patients and their caregivers, including:
These dementia care toolkits can be used by relatives, other caregivers, or those on the staff of busy skilled nursing facilities. These resources are packaged in a container made to fit by a bed or chair and is easily stored.
Finding a way to help those around the patient interact naturally and normally is critical in allowing the patient to retain function and, most importantly, dignity. Our staff’s training enhances skills required to meet the pressing physical and emotional needs of hospice dementia patients.

There is much more that can be written or read about cognitive decline at the end of life, but our goal here is merely to introduce some new concepts in dementia care, and to urge you to contact us if you or someone you love might benefit from Magnolia Care. It’s all part of what makes The Connecticut Hospice such a vital resource to both those we serve, and to the field as a whole.
As we close in on our fiftieth anniversary, we are trying, more than ever, to educate, serve, and advocate for those suffering from life-limiting illness. This is our latest milestone. We at The Connecticut Hospice are here to help.
As a not-for-profit, we depend on generous donors to help us provide customized services and therapies that aren’t completely covered by Medicaid, Medicare, or private insurance.
Please make a gift to help us sustain the highest standard of care.
Admissions may be scheduled seven days a week.
Call our Centralized Intake Department: (203) 315-7540.