Please view our updated COVID-19 guidelines and visiting procedures →.

Food is thought to be one of life’s greatest pleasures. Most of us equate food as a means to nurture and show love. To share a meal is to have a sense of togetherness. We know that nutrients from the food we consume are used to build muscle, provide energy, and most simply, enable all our bodies’ intricate processes to occur. For patients that are nearing the end of life, it is often hard to recognize and accept that the body does not require, nor can it utilize, the nutrients from food the way it once did.
End of life does not indicate a patient’s age or illness, but rather the nearing of the end of a patient’s life. This stage can be the result of a serious chronic illness, such as; heart disease, cancer, stroke, dementia, diabetes, or an accidental injury. Typically, when a patient is initially diagnosed with a serious chronic illness, the patient receives Palliative Care, which focuses on relief of symptoms and stress as a result of the serious illness. Dietary changes may be necessary, but food remains a major source of nutrition and health for the patient.
When a patient is known to be in the end of life stage, they most likely would be receiving hospice care. Hospice Care differs from Palliative Care in that life expectancy is six months or less. Some patients accept their terminal prognosis and begin receiving hospice care immediately, while others chose to continue pursuing a curative treatment. When hospice care does begin, the focus on food and nutrition changes dramatically.
Throughout life the body works hard to grow, build and repair, but the opposite happens at the end of life. The body focuses on transitioning to shutting the processes down, thus requiring less in the way of nutrition. When Connecticut Hospice starts providing hospice care to a patient, whether at its inpatient facility in Branford, in a patient’s home, be it a private residence or another facility, dietary support is an additional discipline that can be beneficial to both patients and family members.
Understandably, there are often many questions and concerns surrounding food and nutrition at the end of life. Concerns over the possibility of “starvation” or “dehydration” are quite common. Dietary care at the end of life can be confusing and unsettling to many. It is often hard for loved ones to recognize that certain conditions may not be “fixed’ or “cured” through good nutrition in a terminal illness. Meeting loved ones where they are on their journey and recognizing how appetite and the ability to eat may change can be an invaluable tool to have. Connecticut Hospice’s Dietary Support staff helps to educate families on these changes and assists in navigating the best way to support their loved ones.
Understandably these concerns can lead to a great deal of distress for the patient and family, and they often find themselves spending much of their limited time worrying, bargaining and at times arguing over food. It is helpful to know that patients at the very end of life do not experience hunger and thirst the way they once did.

At this stage, it is important to educate the family members and/or caregiver on the changes their loved one is going through nutritionally. The enormous amount of energy once needed to process and digest food is no longer required for terminally ill patients. Oftentimes these processes are already strained due to the body’s condition or diagnosis. Forcing foods and/or fluids into the system can produce added stress on the body systems. Nausea, vomiting, bloating, and abdominal discomfort are just a few symptoms that patients may experience when foods or fluids are forced at end of life.
“As hard as it may be, we encourage families to follow their loved one’s cues surrounding foods and fluids at the end of life,” says Connecticut Hospice’s Dietary Support Team member, Alycia Mulhern, RD.

By refusing to eat or drink, the patient is communicating that they are not feeling hunger or thirst and are more comfortable without it. The Dietary Support Team at Connecticut Hospice makes themselves available to answer questions from family members to help lessen fears and anxiety during an already stressful time.
It is the hope of the Dietary Support Team at Connecticut Hospice that by following these recommendations as a guide, it will allow families to spend precious time with loved ones without unnecessary pressure on food and eating. Sitting together holding hands, listening to music, reading a book, or watching a program together are all great ways to feel close and enjoy each other’s company.

In some cases, a patient who is not eating will still want to be part of a gathering that includes food. Recently, Connecticut Hospice held a 100th birthday party for a home care patient. He was smiling ear to ear and had no cake. It is all about meeting the patient where they are.
At the end of life, the goal for loved ones is to transition peacefully, and as comfortably as possible. This includes honoring patients’ preferences when it comes to foods and fluids. It also means trusting that they know their bodies and are doing what it takes to make their process and quality of life the most comfortable while they transition.

The biggest surprise to most people who enroll relatives in Home Hospice Care is that the care isn’t 24/7. In fact, the care is about ten or so hours per week, meaning that the patient’s family is really the main caregiving unit. Still, many services are offered, and understanding how best to engage with the hospice team is very important in working smoothly together to provide excellent end-of-life care.
It is extremely helpful to everyone if the patient enters hospice care more than hours or days before death. Many of the care offered—social work, spiritual care, and volunteer assistance—is unable to be given if the patient is actively dying at the time of admission. See our list of ready signals to help decide, "When's the right time for hospice care?"
Since that admission is prompted by a physician referral, the family should initiate that conversation with the primary care provider, or the specialist, if the topic has not arisen, and active curative treatment is coming to an end. Asking what a doctor might recommend to a relative is often a good way to open the communication channel in a way that allows professionals to give an opinion without seeming too directive.

Once the referral has been received by the hospice organization, an assessment will be done by a medical professional, usually a nurse. That initial visit can take place in a hospital, a nursing home, or a residence. The admissions visit can take a couple of hours, and families should feel free to ask whatever questions are on their minds.
No information about the patient is too trivial to convey, as the more the team knows, the better they can customize care for that patient. Social work and spiritual care will also be in touch for first visits. They can address many issues that might be on the minds of the family, and can help with financial planning, funeral services, or any part of the grieving process.

Once the patient has been entered into service, a routine is usually established. Home health aides may be engaged to help with everyday tasks, such as bathing, grooming, or feeding. While exact timing requests cannot always be honored, due to staffing issues, every effort is made to provide help in the part of the day when it would be most useful. The case manager, who is usually a registered nurse, comes less often than the LPNs and aides, and is frequently juggling many families at the same time, so don’t be surprised if arrival times need to be flexible. It often helps to remember that your needs will be addressed once they are present, and that others may wait when you have a pressing issue.
Because the team members are busy—and that is no surprise, given what we all know about the shortages in all parts of the medical field since the start of the pandemic—families may be hesitant to call between visits. Nurses and supervisors are all adamant that patients and families should be encouraged to call with questions, especially when there have been changes in the patient’s condition. Knowing what to look for is crucial in being able to stop problems before they become bigger, and having them in the medical record early can make a big difference to everyone.
Another important time to call the care team is for medication questions or errors. No issue is too small, whether it be a missed dose or uncertainty about whether the dose was ingested, to avoid calling. Addressing symptoms is one of the main goals of hospice care, and being able to do that sooner is in everyone’s best interest.
In extreme weather conditions, whether it is a winter blizzard or a summer storm leading to power outages, the hospice team will try as best they can, to provide what might be needed ahead of time. Should there be reasons to worry about patient safety during a storm, they can arrange for transfer to an inpatient facility for respite care.

Respite Care can also be accessed for caregiver relief or breakdown. If a family member who is primary in the caring process is sick, away, or unable to cope with symptoms of the patient, respite care in an inpatient facility is available for up to five days. This is an important safety outlet for the exhausted family members, and should be discussed with the home hospice team if it is necessary.

Although home hospice care is given when the “normal course of the illness, untreated” would result in death within six months, many patients in fact outlive that prognosis, sometimes for years. Home hospice care is designed to improve the quality of life, and sometimes that results in an extension of that life span. In those cases, a doctor or an APRN is sent to recertify the patient at various points in the care. Your team will arrange that home visit, which is referred to as a FTF, or face-to-face.
Once the end of life approaches, the team will make sure that you know how to use the emergency drugs in the care package provided for you. Again, do not hesitate to call if you are unclear later as to the proper administration of those medications, or about any other signs or symptoms you might observe. You will be told, and given materials to remind you, that you do not need to call 911. An emergency visit by EMTs will result in lifesaving measures that you may not want, and will very likely land the patient in an emergency room, and sometimes facing a hospital stay. It can be hard, but honoring someone’s DNR (Do Not Resuscitate) request will provide the patient with the final location of his or her choice.
If the patient passes away, call the number provided by the hospice, who will come out and make the pronouncement. Your hospice team will be on hand as soon as is possible, to help with any immediate issues, and will later assist in getting the equipment removed and disposing of medications. Bereavement services will also be provided for thirteen months to the surviving family.
This article is meant to address common issues and questions that arise in the course of providing home hospice care. If there is one thing to take away, it is to call the hospice with any concerns, whenever that may be. Support is a major component of hospice care, and providers are there to guide you through what is an emotionally difficult transition, with expertise and comfort.

One of the most surprising things about the hospice field is that most people have no idea that it is largely funded by Medicare. The Connecticut Hospice was the driver behind, and first recipient of, Medicare funding in 1983. We have a photograph of President Reagan signing the bill. Needless to say, a new era dawned that day. Today, we receive over 90% of our funds from either Medicare or Medicaid.
Because of this healthcare reform, hospice care is no longer something that only the rich can access. In fact, people without strong support systems and safe situations at home are among the most likely to choose to enter hospice care.
Another little-known aspect of hospice care is that coverage is dependent upon certification of terminal illness, which means that a physician has signed that the patient’s disease, with a “normal trajectory”, would lead to death within six months. Clearly, doctors don’t have magic wands, and don’t know exactly how long a patient has to live. They must revisit that opinion after ninety days, and every sixty days thereafter. Some patients live far longer than the first prediction, and some pass away much more quickly.

Another surprise to us is that the six-month period was chosen at random, when the bill was being designed. Many professionals in the field feel that more patients could be helped, at a lower cost to society, if that arbitrary time limit were not imposed. We know, and it should be obvious, that it carries a heavy psychological burden, and deters people who should choose hospice care from doing so. Currently, there are efforts being made to have that set point extended. In the meantime, however, there are still many, many reasons to choose hospice care for yourself or a loved one.
People who do not choose hospice care often get their help from a less comprehensive program, also covered by Medicare, that is called palliative care, or home health care.
Palliative care is meant for those who are recovering from an illness, or going through treatment, and who need help during that period with the daily activities of life. They also must be enrolled formally into such a program, but are intended to be discharged at some point, when their condition improves.
Agencies who provide palliative care are measured by the Center for Medicare Services (CMS) on the improvement in functionality of the patients served. If patients choose this program over hospice care, it often results in poor ratings for the provider, since there would be no improvement—often, quite the contrary occurs.
If a family chooses the palliative, or home health care option, there are some goals similar to those for home hospice care. Those revolve around reducing hospitalizations, or at least the length of stay, allowing the patient to remain in the home (or skilled nursing facility or assisted living facility), and an interdisciplinary approach to care, meaning that social and spiritual services are wrapped around the care given by varying levels of clinicians. Patients are expected, with this service, to be largely homebound.
Should a family feel that they need more services, they should definitely consider home hospice care. If the two programs are presented without names attached, almost everyone votes for hospice care. In addition to the benefits listed above for both types of care, hospice home care layers on additional items that add substantially to savings for the family unit.

When a patient enrolls in home hospice care, they agree to stop curative treatment for the terminal illness, although they are no longer required to be homebound. The reason for the provision for no further curative treatment is that almost all costs, from the point of entry, are covered by the provider agency. Skilled and personal care, medications related to the diagnosis, medical equipment and supplies, and ambulance transportation are all part of this package, in addition to the other professional involvement of social workers, bereavement counsellors, and pastoral care. A team consisting of those listed above, plus speech, occupational, and physical therapists, dieticians, and certified nursing assistants are all involved in setting the plan of care, and available as needed.
Other levels of service can be accessed when necessary under the hospice benefit, including up to five days of inpatient care for management of symptoms or caregiver breakdown. There is also a greater level of home intervention called continuous care, when more hours of home care are needed to handle symptoms or care. Those latter visits can be scheduled for up to 24 hours, if medically necessary. These two types are also included as part of Medicare hospice benefits.
Numerous studies have shown a longer length of “good days”, as well as, in many cases, more days in total, with home hospice care in place of aggressive treatment. There should be no more debilitating ER or hospital stays, no drug side effects, or onerous radiation or surgery. These results are so compelling to many experts that there is now consideration of allowing some treatment at the same time as hospice care, since the overall improvement in quality of life comes on top of the systemic savings from all of the added, and often fruitless, medical care for disease elimination.
When a family makes the decision to enter a patient into any type of care covered by Medicare benefits, whether it be inpatient or at home, they will be provided with paperwork to “elect” the Medicare hospice benefit, by someone who can explain all of the above material.

We all want the best in end of life care for ourselves and our loved ones. The first step in choosing what is right for an individual is to understand the various options. Although they are not unduly complicated, there is a vast amount of misunderstanding and not enough comprehension of what is provided through a patient’s governmental benefits. Hospices can even make the mistake of assuming knowledge that decision makers don’t have, and no one should feel that they can’t receive help with their choices.
Because events often unfold with unexpected rapidity, the best course of action is to thoroughly explore those options ahead of time, and make a plan for the future that best addresses your anticipated, and unanticipated, needs.
We are here to help. Please feel free to contact our Admissions office at any time, either at [email protected], or at 203-315-5740.

“Palliative Care is specialized medical care for people with serious illness, focused on providing relief from the symptoms and stress of the illness. The goal is to improve quality of life for the patient and the family. Palliative care is an essential part of the care of anyone with a serious illness, including people who are continuing to be actively treated, and can not only help people get relief from symptoms like pain and shortness of breath, but also help them to better understand their illness and its treatment so they can choose the care that is right for them -- from ongoing active treatment to hospice.
Palliative care is different from hospice care because it is appropriate for people who are seriously ill and are continuing treatment. With exceptions, such as continuing routine medications for problems like high blood pressure or diabetes, people in hospice care are no longer being treated for serious or terminal illness. For example, people in hospice care are not treated with chemotherapy or radiation for cancer, and focus instead on the relief of symptoms.”
Joseph Sacco, Chief Medical Officer, The Connecticut Hospice

The terms “palliative care” and “hospice” are often used interchangeably, confusing patients and families alike. Many hospitals now offer palliative care services to those in pain. Some are in hospice care as well, some are having active treatment for their diseases, and some are only receiving palliative care for pain management.
Those of us in the field are often guilty of this confusion as well. Often, people who are resistant to the term “hospice”, but are past the point of curative care, are referred for palliative care instead, either to a home health agency or to a home hospice agency.
We have traditionally provided both palliative and hospices of care at the Connecticut Hospice, but have found that, almost without exception, the level of services is fairly comparable. For this reason, we have begun limiting the intake of palliative care patients, as we are judged by CMS, (Centers for Medicare & Medicaid Services) by their level of functional improvement.
Since many are at or near the end of life, little progress in the tasks of daily living is achieved, causing us to get very few stars in the government’s rating system. Hence our hesitancy in taking on patients with whom we cannot succeed, by the Federal definition, yet who truly need our help and care. This is a problem that needs addressing, both by the Federal government, and by physicians. Busy doctors are more likely to suggest palliative care, because it doesn’t carry the weighted overtones of “hospice”.

All of this overlap really goes back to the original Medicare definition of hospice eligibility, which was apparently set more or less randomly at six months of life expectancy at the normal disease trajectory. While that may mean very little in the case of an individual, it has become a catchphrase for our industry, depriving those who cannot be certified of important services, and deterring others who are loath to accept an arbitrary six-month prognosis.
Those of us in the hospice line of business believe that it’s past time to change that standard since the evidence is clear that many, if not most, hospice patients have their lives extended with the skilled and compassionate care that hospice workers give. In addition, people in the care of home hospice are frequently able to avoid or minimize time spent in hospitals and urgent care settings, which patients find very taxing and debilitating, without even considering the expense of multiple hospitalizations. If the time frame being discussed were twelve or eighteen months, more patients would likely choose home hospice, and possibly live as long or longer than with aggressive treatment.

The issue of continuing treatment is complicated and also seems to be transitioning. There are many patients who continue to seek treatment for their disease because they can, and, even if it’s a long shot, they don’t want to stop. Since hospice care is considered to be CMO (comfort measures only), and since hospices are required to pay for all treatment and equipment related to the patient’s diagnosis under hospice care rules, this means that we can’t afford to take someone who is undergoing treatment.
Palliative care is compensated at a much lower rate, meaning that caring for a very ill patient continuing treatment, but needing end of life care, doesn’t make financial sense for a home care agency, if that means that they are providing hospice level care, but being paid for routine palliative care. A terminal patient still having treatment is just as sick, or sicker than, a patient receiving comfort measures only, yet the payment for palliative care is far less than for hospice care. In the case of hospice care, even if an exception is made for certain types of treatment, the expense of that treatment puts it out of reach for hospice budgets.
When deciding on care for a loved one, all of these factors can come into play. It’s hard to discontinue treatment from an emotional point of view, even if it is causing side effects (although newer infusion therapies and immunotherapies are much more likely to be tolerated easily). Also, doctors are taught to cure, not to counsel acceptance of death. However, many patients live fuller, and even longer, lives when symptoms are managed and care is compassionate but not meant to be curative.
This is where the confusion of terms comes in: We would consider that symptom management is both hospice care and palliative care. From a home care billing point of view, however, the two are separate, with palliative care used to mean care for a serious illness where improvement is expected, and hospice care used to mean care for the same illness, once the goal of curing the disease has been foregone. To confuse matters further, Palliative care in hospitals can be “comfort measures only”, which is technically hospice care, or pain management. It’s no wonder that families get confused!
The most important starting point is for the patient and his/her support team to have an honest conversation among themselves, and with their treating physicians, about the effectiveness of current and future treatment, a true prognosis for the disease at hand, and the goals for that person’s life trajectory. Some will choose length of life, some will choose quality of life. Sadly, it often happens that assumptions are made, or hard truths are not voiced, so that treatment and care can be working at cross purposes.

If treatment is still desired, a hospitalized patient may still see a palliative care doctor, but the medical team’s efforts are aimed at gaining a cure, or a remission, of the illness. In many cases, this aim means that the patient may have more discomfort, both from the disease and from the treatment. Doctors also can’t know for sure how different people will be able to tolerate, or not, various regimens for treatment. Often, it is not clear early on whether treatment will work, so all of these factors need to be revisited regularly.
When a patient and his/her family come to the decision that comfort care is the way to go, our full attention can be mobilized in that direction. After decades of experience, we have become experts in delivering care whose aim is to fulfill wishes, promote comfort and closure, and relieve pain. Since our goals are less long term, tolerable pain levels are often left to the patient; he/she might choose to remain more lucid, albeit with discomfort, or to be more sedated and have more relief.
It should be clear by now that the patient and family are at the center of this choice, as they should be. All people should be given enough information to make the decisions that are in their own best interests. In fact, that was a primary reason for our founder, Florence Wald, to establish The Connecticut Hospice as the country’s first hospice. She believed passionately that patients and their families needed to be considered as a unit, and that they should be given their diagnoses and prognoses, which wasn’t commonly done fifty years ago. She trusted in the innate wisdom of those at the end of their lives to decide how to spend their remaining days, months, or years, and in the ability of nurses and other medical professionals to help those wishes to come true. And that is as true today at The Connecticut Hospice as it was at our inception.



Having seen tens of thousands of patients over the past five decades, The Connecticut Hospice has the highest amount of professional skills for end-of-life care management. Over time, The Connecticut Hospice has progressed from its original beginnings—providing care for cancer patients and their families—into serving all patients, regardless of diagnosis. One of the conditions which has seen a huge increase in incidence is dementia, in part because other diseases can be cured or controlled, leaving more people to suffer from mental decline at the end of life. This can be particularly hard on families, who are often grieving the loss of the person they knew, while that loved one is still alive. Our new program, Magnolia Care, will increase the services and support to patients and families with Alzheimer’s disease, and other cognitive failures.
The training that we are giving to our nurses, aides, and social workers, combined with our longstanding knowledge of treatment options that preserve quality of life, has allowed us to design Magnolia Care in the most thoughtful of ways. In order to best understand what we are offering, it will help to provide some explanation of the progression of dementia.


Between 5 and 8% of the U.S. population over 65 is living with some form of dementia, with that number rising to 50% of those over 85. Dementia is defined as cognitive changes that affect thinking, personality, and behavior. It can be difficult to diagnose in its earlier stages and can be confused with other causes of those same symptoms. However, it occurs broadly across these age groups and is expected to increase as life expectancy rises and more people enter this demographic.
Early phases of the disease can often be managed by families without outside support. Minor adjustments in daily living arrangements, or additive monitoring of complex tasks, can suffice for some period of time. Independent living may be a challenge but is sometimes prolonged with enough support from relatives or paid caregivers.
The final stage of most diseases of dementia occurs between 3 and 6 years after a diagnosis is made. The progression of the disease does not follow a specific timeline and is different in each case.
This period of advanced symptoms may be months or years in length and could include a variable course of events which is unpredictable. Regardless of the type of dementia, there are some typical features that are often common at this time:
Magnolia Care is designed specifically for persons living with dementia at the end of life. Nurses, social workers, chaplains, nurse aides, art and music therapists, and volunteers all undergo intensive training and are certified in person-centered dementia care and non-pharmacological interventions.
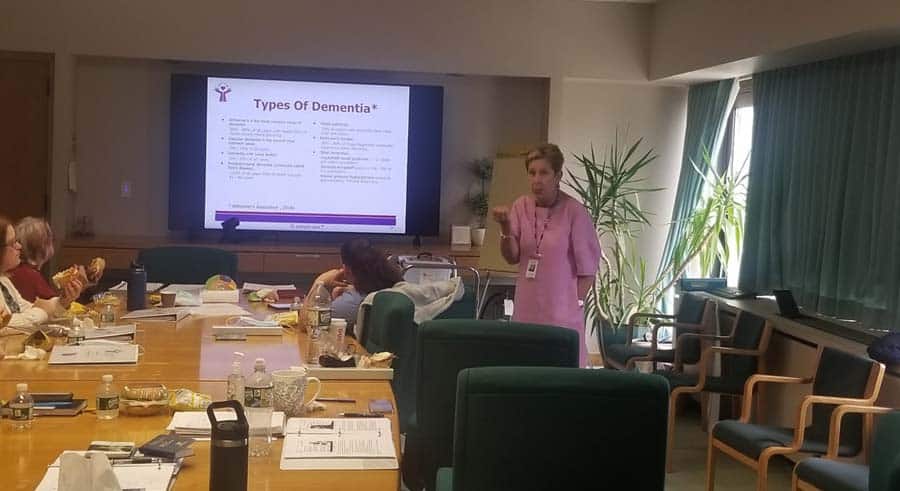
Our final-stage dementia care training was created by a hospice nurse with extensive experience caring for patients with dementia. This dementia-expert-lead training focuses on the behaviors and needs of hospice patients with cognitive failure, ensuring that Connecticut Hospice caregivers can recognize and respond to the concerns of dementia patients and families.
Like all of our Hospice Care programs, Magnolia Care provides a comprehensive approach that incorporates all the members of the hospice team in a plan of care that addresses the unique needs of each patient.
We have assembled a “tool kit” for use in homes, nursing homes, or assisted living, which offers enhanced tools for the management of symptoms, and can allow patients to access deeper memories, providing both solace and joy. The goals are to reach those patients where they are in their journey, help families to communicate and comfort their loved ones, and reduce the need for pharmacological solutions to common problems with behaviors.
Music is a known soother of dementia symptoms, and we work with caregivers to provide appropriate and significant music, tailored to the individual’s taste and age. MP3 players are embedded with this music in teddy bears, comfortably used by even people who are cognitively impaired.

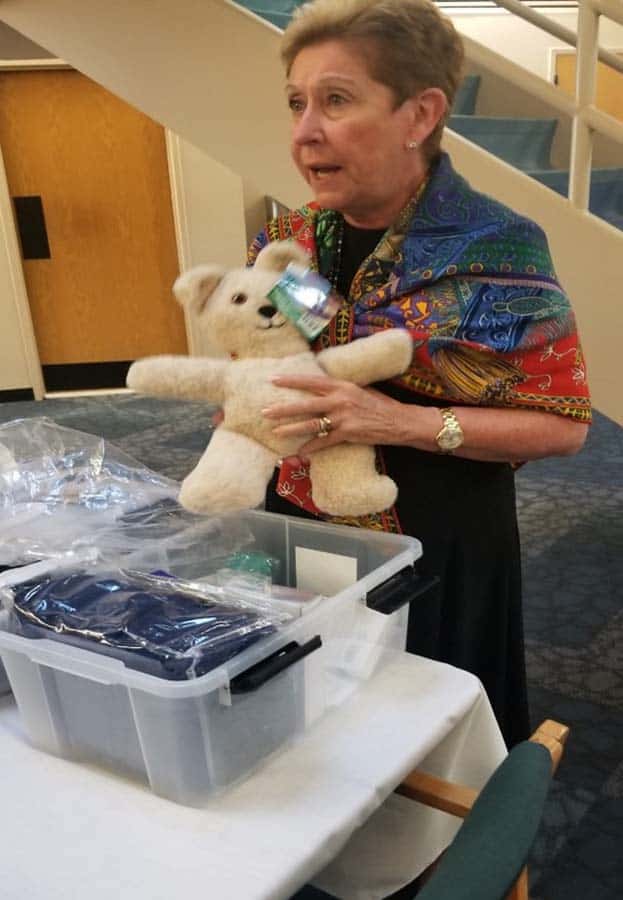
The toolkits also include a diverse range of items to help dementia patients and their caregivers, including:
These dementia care toolkits can be used by relatives, other caregivers, or those on the staff of busy skilled nursing facilities. These resources are packaged in a container made to fit by a bed or chair and is easily stored.
Finding a way to help those around the patient interact naturally and normally is critical in allowing the patient to retain function and, most importantly, dignity. Our staff’s training enhances skills required to meet the pressing physical and emotional needs of hospice dementia patients.

There is much more that can be written or read about cognitive decline at the end of life, but our goal here is merely to introduce some new concepts in dementia care, and to urge you to contact us if you or someone you love might benefit from Magnolia Care. It’s all part of what makes The Connecticut Hospice such a vital resource to both those we serve, and to the field as a whole.
As we close in on our fiftieth anniversary, we are trying, more than ever, to educate, serve, and advocate for those suffering from life-limiting illness. This is our latest milestone. We at The Connecticut Hospice are here to help.

In many parts of the country, people think of hospice care as home care, where nurses come into private homes and help caregivers take care of end of life patients. In our area, Connecticut Hospice’s large inpatient facility brings GIP (general inpatient) to families as well. But hospice care is not just provided in hospices, or in homes. It can be delivered in any setting where a patient lives.
When someone moves to a skilled nursing facility(SNF) or assisted living, that becomes the patient’s home, and home hospice can assist there. For nursing homes, especially, this can be a great boon for families. Especially during the pandemic, much has been written about staffing shortages at SNFs. Hospice nurses and aides can supplement the care given by a skilled nursing facility.
For example, eating can become an issue for people with certain conditions. Sometimes, carefully feeding by trained professionals can increase their caloric intake significantly. Very few places would have the ability to feed many patients that way, but home hospice care can bridge the gap. Often, aide service is requested during mealtimes, and supplements the resources available for meal assistance.

Personal care is another function of daily living that can become problematic, especially with dementia. Patients can become resistant to bathing, or may need time-consuming help with dental maintenance. Again, home hospice aides may be used to add extra resources for those aspects of ongoing support.


At Connecticut Hospice, we have trained all of our home care staff in special techniques to improve the quality of life for patients with dementia. There are methods for feeding, bathing, and other activities that will improve the outcomes for those who can receive such personal attention.

If a patient is accepted as appropriate for home hospice care, he or she becomes eligible for Medicare Hospice Benefits (MHB). Those benefits are specified by Medicare, which pays for most of the hospice care delivered across the country. There are certain parameters for entry into that service, and someone must be referred by a physician. At that point, he or she would be evaluated by a hospice service, and, if appropriate, can then be admitted for MHB.
This can take place in any setting. A patient residing in a skilled nursing facility would be visited there by a hospice representative, and then enrolled in that setting.
Or, a patient can be released from an inpatient hospital or hospice setting, and sent home or to a SNF or Assisted Living Facility (ALF) with home hospice care. Evaluation can take place before the patient is discharged, so that all necessary equipment and medications can be delivered before the patient gets to the next setting.

Home hospice care covers the cost of those medications, as well as the equipment needed. Routine home care does not provide that level of assistance. Sometimes, patients and families resist the use of hospice care, just because of the word “hospice”. Before declining such help, people should understand that Medicare Hospice Benefits are a component of Medicare, and that the financial implications can be great, depending upon the level of care authorized for a recipient.
Accepting hospice home care does not put a time limit on someone’s life, but it does mean that the normal trajectory of an illness would indicate an expected lifespan of less than six months, in the opinion of a referring physician. It also means that they are no longer seeking curative treatment for an illness. We call this “comfort care”, as opposed to active methods of fighting the disease. There is a great range of outcomes with this type of care, but many people live longer. If you need help deciding about when’s the right time for hospice care, we have a list of ready signals that you can discuss with your physician.
Since curative treatment can be debilitating, hospital stays generally take a toll on the patient. Careful management of symptoms, especially pain, is a hallmark of hospice care, and one that can lead to a better quality of life. That in and of itself can prolong a person’s “good” time, and improve his or her outlook. It does not, therefore, necessarily indicate defeat, or failure, to choose hospice care. There are many good reasons to consider comfort care in a safe and supportive setting.

Understanding the finances behind Medicare Hospice Benefits is also key to peace of mind. In a nursing home setting, the family either pays for room and board, or is covered by insurance or Medicaid, depending upon the level of assets a patient has. The extra care provided by a hospice is paid for by Medicare, directly to the hospice.
Even in assisted living, where usually an upfront cost has been paid by a patient, in order to cover whatever services are necessary, hospice care is covered by Medicare, if the person is referred and deemed appropriate. The rules about visitation and distribution of medications can be different, but the concept is the same. Again, the hospice is paid directly by the Center for Medicare Services, as it would be in a private home.
It’s worth a word at this point about virtual hospice in a hospital. If a family member is too ill to transfer to home or even an inpatient hospice setting, end of life services can be provided in a traditional hospice environment. In those cases, the referring hospital would call in a hospice, and it would admit the patient and provide services in the hospital bed.
The hospice pays room and board in those cases to the hospital, but the patient and his or her family is not involved in that process, nor is the family responsible for paying for the extra services of hospice personnel. Not all hospitals have such an arrangement with individual hospices, but it is worth asking to see whether that is an option in any particular case.

For those patients on private insurance, they are also generally available, and the hospice can check for authorization. Also important to remember is that those services can be additive, so that they supplement whatever care is being given already, and provide additional comfort and aid to caregivers.
One of the goals of comfort care is to ensure that patients receive adequate pain relief and symptom support. This alone can lengthen and/or improve life. Another consideration is the reduction of hospital time—if hospice care prevents additional hospitalizations, or reduces the length of stay, it’s understandable why Medicare would pay for it. Caregivers are taught to call hospice before dialing 911, because sometimes episodes can be managed without a trip to the emergency room.
There are resources available to assist patients and families along the journey of an illness, and they are both easily accessible and affordable. As the country’s first hospice, we know well the need for our services, and hope to help others access them whenever appropriate.
Learn more about hospice care, and its many settings.
As a not-for-profit, we depend on generous donors to help us provide customized services and therapies that aren’t completely covered by Medicaid, Medicare, or private insurance.
Please make a gift to help us sustain the highest standard of care.
Admissions may be scheduled seven days a week.
Call our Centralized Intake Department: (203) 315-7540.